
Mission: A Faster, Better MRI
Magnetic resonance imaging (MRI) is a gold standard tool for capturing crisp, detailed pictures without radiation, to diagnose serious conditions like cancer and epilepsy.
But to Dan Ma, PhD, associate professor of neurosurgery and associate professor in biomedical engineering, it’s still too imprecise.
She compares it to checking for a fever by touching someone’s forehead: useful, but subjective. “When radiologists read clinical MRI images, they will say a lesion is brighter or darker compared to another area,” Ma said. “It’s a very qualitative evaluation. It’s not giving you an absolute value measuring tissue property.”
In addition, results can differ depending on the scanner or even the day. “There’s no standard way of showing an image,” Ma said. “Even at the same scanner, on a different day, the image contrast may be a little bit different.”
In 2013, while still a PhD student at Case Western Reserve University, Ma introduced a better solution: MR fingerprinting. Like using a thermometer instead of a hand, this method assigns objective numbers to tissue properties. And because of the way the images are gathered, the scans are faster (good news for anyone who’s endured the claustrophobia of lying inside an MRI machine for half an hour).
"Dr. Ma is a brilliant biomedical engineer in neurosurgery who is redefining what’s possible with brain imaging. MR fingerprinting is the kind of neuro-innovation that directly impacts patient care."
- Gerry Grant, MD, professor and chair of neurosurgery
Ma and colleagues, including her mentor Mark A. Griswold, PhD, published the details of their invention that same year in the journal Nature.
Ma has been working with imaging company Siemens to take MRI fingerprinting to market. In 2023, the technology reached a big milestone — Food and Drug Administration approval. “It’s clinically ready,” she said. “In five minutes, you can scan the entire brain."
In January, Ma left a faculty position at Case Western Reserve University to join Duke University School of Medicine, and she is excited about the move and the potential to focus on image-guided treatment.
Gerald Grant, MD, the Allan H. Friedman Distinguished Professor of Neurosurgery and chair of the Department of Neurosurgery, said that Ma’s work with MR fingerprinting has to potential to transform how doctors detect and treat conditions like brain tumors and epilepsy.
“Dr. Ma is a brilliant biomedical engineer in neurosurgery who is redefining what’s possible with brain imaging,” he said. “MR fingerprinting is the kind of neuro-innovation that directly impacts patient care. We are very proud to have her advancing this exciting work here at Duke.”

Random But Precise
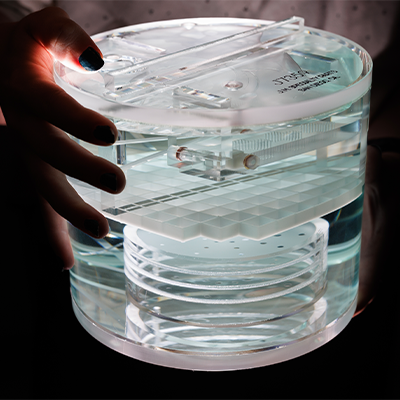
While traditional MRI acquires images step-by-step, measuring one tissue property at a time, MR fingerprinting gathers data more randomly but from a single scan. It varies scan settings (like flip angle and phase or radiofrequency pulses) to capture a wide range of signals all at once. These signals form unique patterns, like fingerprints, that help identify different types of tissue more precisely and consistently.
After the scan, a computer algorithm compares the "fingerprints" from a particular patient to a “dictionary” of all theoretically possible patterns. By finding the best match, it can figure out the exact properties of the patient’s tissue, including the presence of tumors or other abnormalities, Ma said.
The beauty of MR fingerprinting is its built-in tolerance for error. Scanning for patterns, rather than complete pictures, means a test that’s faster and easier for patients. Imagine getting an MRI and not having to lie completely still. This feature may also reduce the need for super-high-resolution scanners, which could translate to lower costs.
“It’s similar to human fingerprints at a crime scene,” Ma said. “You may get just partial fingerprints. But you can still find the suspect because you have a powerful algorithm to extract information from those imperfect fingerprints.”
The challenge now is to perfect the technology for incorporation into commercial clinical machines that could be used widely in patient care. “It has to be robust across many different clinical scenarios: different types of patients, scanner imperfections across different sites,” Ma said.
Backed by National Institutes of Health funding and powered by MR fingerprinting technology, she is on a mission to make diagnosis and treatment easier and more accurate for epilepsy, brain tumors, breast cancer, and prostate cancer.
For patients with focal cortical dysplasia— a form of epilepsy often missed by standard MRI — Ma is working to uncover hidden lesions, opening the door to life-changing surgeries and seizure-free lives. In breast cancer, she’s using imaging to detect whether chemotherapy is working before treatment ends. As she puts it, “Why keep giving chemotherapy if it’s not working?” And for men with suspected prostate cancer, her goal is clear: fewer unnecessary biopsies, thanks to AI-driven imaging analysis and new, objective biomarkers.
Ma said that her move to Duke is key to her future success in making MR fingerprinting a more routine part of clinical diagnosis and treatment. “Duke Neurosurgery is the best place,” she said. “They have great patient resources and expertise on how to treat neurological diseases, and the world-renowned brain tumor center.”
Angela Spivey is assistant director of editorial in the Office of Strategic Communications at Duke University School of Medicine.
Eamon Queeney is assistant director of multimedia in the Office Strategic Communications at the Duke University School of Medicine.
