
Looking for the Achilles’ Heel in Treatment-Resistant Tumors
While cancer treatment has come a long way, Christine Eyler, MD, PhD,isn’t satisfied. “We could do a lot better,” she said. Eyler, the Butler Harris Assistant Professor in Radiation Oncology, hopes her research will help find more effective ways to vanquish tumors.
She examines how tumors change during radiation treatment, with the goal of identifying new targets for therapy.
She researches rectal cancer, which is typically treated with radiation and chemotherapy at the same time. “Tumors may evolve to be more resistant to chemoradiation,” she said, “but it may open up an Achilles’ heel of sorts, where they become increasingly susceptible to another treatment.”
In the future, rectal cancer patients might receive an additional therapy midway through the standard treatment, to take advantage of an Achilles’ heel. “We’re far away from that now,” Eyler said, “but there are reasons to think that might be something we can achieve.”
A Better Way to Study Cancer in the Lab
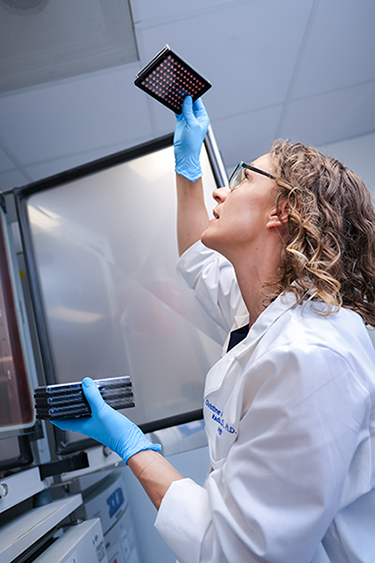
To investigate the changes that tumors go through during treatment, Eyler uses rectal cancer organoids, which are three-dimensional cultures of cells from patients’ tumors. The cells came from rectal cancer biopsies from 20 patients. Organoids, unlike traditional flat cell cultures, contain some of the structural features of real tumors. “That culture method allows them to maintain some of the complexity and heterogeneity that are evident in patients’ tumors,” she said. “I fundamentally believe they are better study models.”
Eyler subjects the organoids to treatments including radiation and chemotherapy and investigates how tumor response changes over time. “The tumor might be responsive at the beginning, but a certain population of cells might survive and have an advantage as the treatment goes on,” she said. “I’m interested in tracking tumor evolution in response to therapy.”
She looks at both genetic changes and epigenetic changes. Genetic changes are differences in the actual genetic code, while epigenetic changes affect how or whether certain genes are expressed. Tumors from different patients will likely respond in different ways, leading to different susceptibilities. In the future, that might translate to personalized treatment based on a patient’s tumor profile.
If Eyler can find some Achilles’ heels in treated rectal tumors, she hopes she’ll be able to develop new treatment strategies and partner with others in the department to evaluate the new strategies in clinical trials.
Looking to Epigenetics for Cancer’s Origins
In addition to studying irradiated rectal cancer, Eyler uses new technology to learn about how epigenetic changes promote cancer growth in the first place. A common type of epigenetic change is called methylation, in which the addition or subtraction of a molecule called methyl influences gene expression.
Another epigenetic player involves the architecture of chromatin, the proteins that form the structural scaffolding for DNA. Changes in the architecture of chromatin can bring certain proteins and genes in a long DNA strand close to one another, influencing whether those genes are expressed. Eyler is using new technology to shine a light on that architecture.
“There’s this whole epigenetic chromatin code that influences the regulation of important genes in normal biology as well as cancer biology,” Eyler said. She suspects that changes in chromatin structure could explain such things as the absence of tumor-suppressing genes in cancerous tumors.
“There are a lot of genes in cancer that get dysregulated – not through mutation or methylation – and we don’t know how or why,” she said. “My hypothesis is that they have altered chromatin structure and regulation.”
Understanding how gene dysregulation leads to cancer could yield important new information about how to stop it. “It’s not a clear, straight path to patient benefit,” she said, “but these are the questions that build the field to be able to make those advances.”
A Roundabout Journey to the Clinic
As an undergraduate at Duke, Eyler planned to pursue a PhD and become a scientist. Those plans changed after she became friends with the son of Henry Friedman, MD, the James B. Powell, Jr. Distinguished Professor of Pediatric Oncology. Friedman had a hunch she would excel as a physician. So, he invited her to shadow him in the clinic.
Eyler already knew she loved science, but she discovered she loved interacting with patients too. That’s how she ended up becoming a physician-scientist, earning her PhD and MD at Duke. “She really captures the concept of physician-scientist,” said Christopher Willett, MD, chair of the Department of Radiation Oncology. “She’s a model clinician and has been highly productive and innovative at an early point in her career.”
Eyler, who describes herself as an “I love everything” person, said the combination of patient care and lab work suits her. And she finds that her clinic days provide the fuel for her lab days. “I get a lot of my drive and motivation from seeing what patients go through,” she said.
Mary-Russell Roberson is a freelance writer living in Durham.
Photos by Huth Photo.
