
Duke Celebrates 50 Years of Cancer Care — and Looks Toward the Next 50
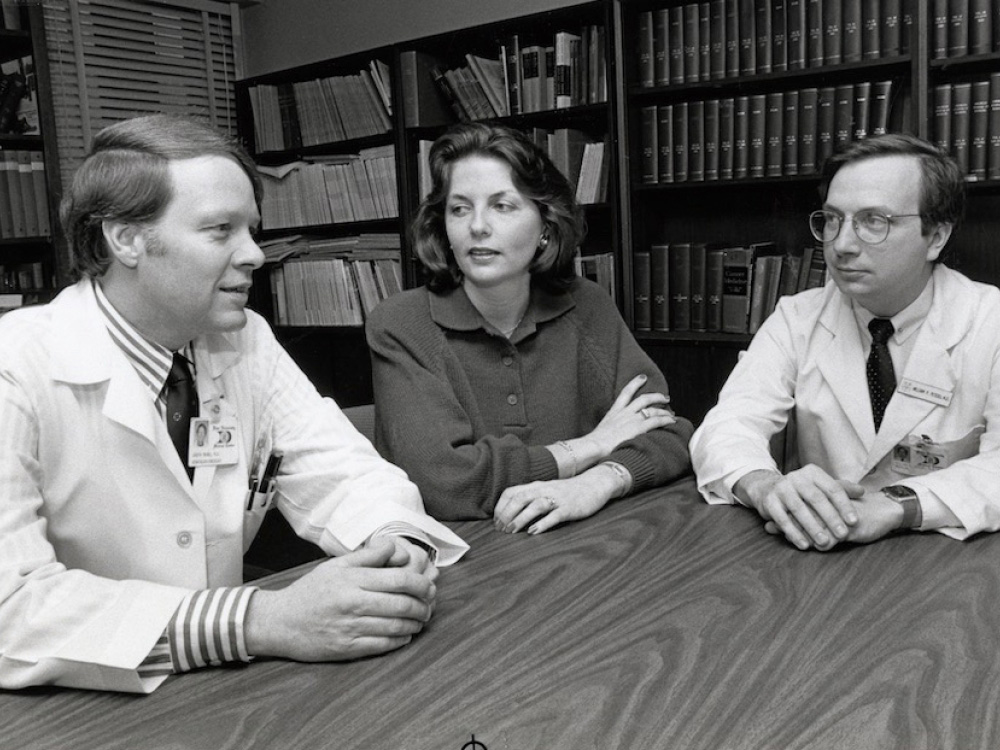
When Joseph O. Moore, MD, came to Duke as a fellow in 1975, he and his mentors treated chronic myeloid leukemia (CML) with a chemotherapy regimen that was like a "wet blanket." It suppressed the cancer for a few years. "But it didn't change the trajectory of the disease," Moore said. Patients developed acute leukemia, which was almost always fatal.
By the early 1990s, younger patients could achieve a cure with a bone marrow transplant, though complications were common. By 1999, Moore was the Duke investigator for a national study of a targeted drug, imatinib, which stops leukemia cells from growing by shutting down a key protein. When imatinib was approved by the Food and Drug Administration (FDA) in 2001, it transformed CML into a disease easily treated by taking a pill.

When Moore retired from clinical practice in 2019, he was involved in a study following people with CML who had been taking imatinib long term, which showed they could safely stop therapy.
The CML example provides a snapshot of just how far cancer treatment has come in the last 50 years. For many patients, "There's an expectation of success and people living normal lives," said Moore, professor emeritus of medicine.
Much of that progress can be traced to research funded by the "war on cancer," which launched in 1971 when congress passed the National Cancer Act. The act gave the National Cancer Institute (NCI) the authority and funds to create a national cancer program. The backbone is a network of comprehensive cancer centers that provide patient care and conduct rigorous research to find new and better ways to prevent, diagnose, and treat cancer.
Duke was one of the original eight such centers, designated in 1973 because of the strong research and clinical care programs it had already put into place, including one of the first brain tumor programs in the United States, said Steven Patierno, PhD, deputy director of today's Duke Cancer Institute (DCI), and professor of medicine.
In fact, one of the advocates for the 1971 National Cancer Act was William Shingleton, MD, the first director of the Duke Comprehensive Cancer Center, as DCI was known in 1973. The chance to work with Shingleton and other research pioneers was one of the reasons that Moore came to Duke for fellowship and stayed on as faculty, he said.
As Duke celebrates its 50th anniversary of transforming cancer discovery and care, researchers and providers envision a future when all cancers are easily treatable; physicians can detect and stop cancer earlier and earlier; and everyone has the same opportunity to survive cancer.
Reducing Toxicity

Surgery, as well as treatments that are toxic to all cells, like standard chemotherapy and radiation, were the first weapons against cancer, and they're still used today. One of Duke's contributions was making chemotherapy easier to tolerate, through clinical studies that led to the FDA approval in 1990 of a growth factor (G-CSF) that stimulates bone marrow recovery, decreasing infections and hospitalizations. "G-CSF is used all over the world now for patients getting chemotherapy," said Michael Kastan, MD, PhD, executive director of Duke Cancer Institute and the William and Jane Shingleton Professor of Pharmacology and Cancer Biology.
Also in the 1990s, Duke made advances in bone marrow transplant, including opening the nation’s first outpatient transplantation program in 1992. High dose chemotherapy is given on an inpatient basis, but bone marrow infusions are performed at outpatient clinics. "Patients did not have to be hospitalized, so they were able to move about more and eat better. The costs tend to be lower as well," said Nelson Chao, MD, MBA, Donald and Elizabeth G. Cooke Professor and chief of Duke’s Division of Hematologic Malignancies and Cellular Therapy.
Today, transplants help many patients with acute leukemias and lymphomas, and the program provides all follow-up care outside the clinic for transplant patients in recovery, at their homes or an apartment near Duke. The team was the first in the world to test this practice in 2014. In 2020, in response to the COVID-19 pandemic, they made it standard of care. The practice reduces the number of people each patient is exposed to and may reduce complications and improve survival, Chao said.
Hitting the Target
Thanks to such advances, the death rate from cancer in the United States has declined every year since 1991, according to the American Cancer Society.
Targeted therapies, which directly "hit" a specific protein or other molecule that has caused cancer to grow, have played a large role in that progress, Kastan said. Imatinib, the drug that Moore studied, was the first targeted therapy. Duke made key contributions in developing other targeted therapies, including Avastin, the first such therapy that worked by shutting off the tumor's blood supply, and lapatinib and trastuzumab, some of the first targeted therapies to treat metastatic breast cancer.
Despite such developments, some cancers still have low survival rates, and there aren't targeted therapies for most tumor types, because research is in "its infancy" in understanding the genetics of tumors, Kastan said. "We'd eventually like to stop using cytotoxic therapies, but that's going to be a long time."
Immunotherapies, which harness the immune system's ability to fight cancer, are another focus for the future. Immunotherapies that emerged beginning in 2010 have led to improved survival times for some cancers, and by 2015 they made it possible for lung cancer patients to achieve long-term survival for the first time, said Scott Antonia, MD, professor of medicine. The DCI Center for Cancer Immunotherapy, which Antonia directs, works to translate Duke discoveries into new immunotherapies, and to make these treatments work better for more patients.
Intercepting Cancer Before it Starts
No matter the treatment, the future of cancer care will continue to move toward precision medicine, or "finding the right treatment for the right patient at the right time," Kastan said. This includes choosing treatments based not only on the genetics of the tumor, but also on the genetics, age, and risk factors of each patient.
Duke has made some inroads with a Molecular Registry of Tumors that stores information about mutations in patients with advanced cancers, uses Duke-created software to match patients with treatments that may work best for their tumor, then notifies doctors automatically. In addition, Duke researchers in prostate cancer and colorectal cancer have in the last three years led clinical trials showing that a "liquid biopsy" can be used to track how tumors are evolving and responding to treatment, Kastan said. Liquid biopsies use a blood test to detect circulating tumor cells or tumor DNA, so they are less invasive and faster than traditional tissue biopsies.
Other researchers envision a time when no one ever develops full-blown cancer. Duke researchers from many different fields are working to develop new methods of "interception" — intervening once someone has started down the "cascade" of events leading to cancer, but before actual cancer develops, said Meira Epplein, PhD, co-leader of the Cancer Risk, Detection, and Interception research program.
For instance, gastroenterologists are practicing interception when they remove pre-cancerous polyps during a colonoscopy. Another example — testing and treating for the stomach bacterium H. pylori, which causes ulcers. A two-week course of antibiotics eradicates the bacterium, reducing stomach cancer risk by 50 percent, Epplein said.
Treating the Person, Not Just the Cancer
Duke was one of the first cancer centers focused on the needs of the patient as a person. In 1987, Rachel Schanberg founded the Duke Cancer Patient Support Program in memory of her daughter, Linda Schanberg Clark, who died from Hodgkin's disease at age 26. "She was the first to say that her daughter received excellent medical care, but she felt there were many challenges for her daughter and her family that no one talked about," says Cheyenne Corbett, PhD, who worked with Schanberg and is now co-director of the Duke Supportive Care and Survivorship Center.

Schanberg quit her job as a school counselor to direct the program. Corbett heard about it in 2002 when she was finishing a doctoral degree in family therapy at Nova Southeastern University in Florida. "Even then, there were very limited options in cancer centers or in the community to help families facing cancer," Corbett said.
Corbett started working with Schanberg in 2002 part time, coordinating volunteers and providing counseling. There was very little money, but Schanberg persisted. "She was one of the strongest, feistiest people I've ever met," Corbett said.
"Every day, if Rachel saw a patient in need or someone who looked lost or confused or sad, she would stop and sit and just connect with them," Corbett said. "That's the heart of what we do: Stop and really listen to what the patient is going through." Corbett became director of the program when Schanberg retired in 2006, and she and her team have grown their cancer support services and research into the DCI Supportive Care and Survivorship Center, created in 2017. The center offers patients and families an array of services, such as therapy, patient navigation, tobacco cessation, a teen and young adult oncology program, financial assistance, exercise consults, a program focused on heart health, a sexual health and intimacy program, a cancer genetics program, and fertility services.
A New Era at Duke
In 2010, then-Chancellor for Health Affairs Victor Dzau, MD, announced plans to unite all of Duke's cancer care, research, and education under one organization — Duke Cancer Institute (DCI). This structure breaks down barriers between departments and between the health system and the university, said Kastan, an accomplished cancer biology researcher who came to Duke in 2011 after leading the cancer center at St Jude's Children's Research Hospital. "I knew that in the setting of this structure, that the sky was the limit, and that we could do great things in this environment with the great people at Duke."
The new investments included a 267,000-square-foot Duke Cancer Center building. It opened in 2012 with natural light, family space, and clinics set up so that patients see multiple providers in one building. Staff and patients worked with architects and designers to make the building "a physical embodiment of Duke Cancer's philosophy of patient-centered care," Corbett said. "That is one of the reasons why it's such a special space; the voices of team members, patients, and families were included in the design."

Working Toward Health Equity
In 2012, after Patierno left his position as founding executive director of the George Washington University Cancer Center to become deputy director of DCI, one of the first things he and Kastan did was launch an Office of Health Equity to improve population health for communities that DCI serves. “Lack of access to care, lack of early detection, lack of healthy lifestyle, lack of education, lack of health insurance, lack of trust in the medical system — all of these things work together, and we need to implement solutions that address all of them,” Patierno said.
In 2017, that team, led by Nadine Barrett, PhD, won an Innovators Award from the American Association for Cancer Research, for their work developing community partnerships to reduce cancer disparities. Those activities include developing a diverse and engaged community advisory council, forming a research agenda, and implementing a program of community-facing navigation and screening events. The team is now part of a larger program called Community Outreach, Engagement, and Equity.
If screening shows that someone needs further care, there are many points where the system can break down, Patierno said. Duke employs people called navigators who try to find and overcome those gaps. The same community-facing navigators who work with people at screening events provide detailed follow-up to arrange treatment, at Duke or even at other cancer centers, depending on the person's location and needs, said Angelo Moore, RN, PhD, assistant director of community outreach, engagement, and equity for DCI.
At Duke, the community-facing navigators make a "warm handoff" to internal patient navigators, who help patients get appointments and connect them to financial services, transportation, and other support. The team continually works to improve and expand this model, which spans pre-treatment through active cancer treatment and survivorship (care after active cancer treatment ends), Patierno said. A paper describing the model was published in April 2020 in Cancer Medicine.
"The ultimate goal is to achieve cancer health equity," Patierno said, which means that everyone would have an equal opportunity to prevent, detect, treat, and survive cancer.
Angela Spivey is a Senior Science Writer in the School of Medicine Office of Strategic Communications.
Illustration by Ken Orvidas.
