
Executive Summary
As a result of an extensive analysis, the following outlines a strategic plan for organizing Climate and Health research led by the Duke School of Medicine.
The analysis encompassed a canvas of research at the intersection of climate and health already underway at Duke, surveyed faculty and trainees to learn about their interests, surveyed external partners, and sought insights by interviewing faculty and leaders at the University and community members outside the University.
It became clear there are key differentiators for Duke in climate and health research, namely its expertise in translating discoveries to implementation, its unique expertise and resources (e.g. the Duke Global Health Institute, the Duke Human Vaccine Institute, the Duke Clinical Translational Science Institute, and access to patient health data), deep ties to local and global communities, and, above all, a collaborative environment that encompasses all Schools within Duke University.
The analysis identified four areas, or themes, where Duke is uniquely placed to become a global leader in Climate and Health research.
- Biology and Physiology of Heat: basic discovery research efforts focused on understanding myriad direct (i.e. physiology, immunology) and indirect effects (i.e. pathogens, nutrition) of heat on human health.
- Climate and Health Observatories: facilitating the development of critical surveillance strategies, technologies, and models to describe and measure how climate change is altering health in climate-vulnerable regions across the globe with a focus on defining effective interventions and public health plans to mitigate their effects.
- Data Solutions for Climate and Health: development of a central data repository and advanced analysis methods to integrate well-curated climate data with local and global human health data thereby allowing investigators to identify trends, establish causal associations, and predict future Climate and Health events.
- Policy and Resilience in a Changing Climate: Policy and strategy developments that build resilience in communities, institutions, and healthcare delivery systems, thereby enhancing adaptive capacities, reducing vulnerabilities, and promoting sustainable development in the face of Climate and Health challenges.
Finally, the analysis focused on resources required to initiate the Climate and Health Research Initiative (CHeRI) and areas to expand efforts and ultimately sustain them through extramural grant funding and philanthropy, including administrative infrastructure, symposium and networking events, funding for startup and existing research activities, community engagement, recruitment and funding for faculty and trainees.
Climate change is the most significant global threat of our time. As our climate changes, we are experiencing more frequent extreme weather events - heat waves, severe storms, and prolonged droughts. Extreme weather causes secondary effects including coastal erosion from sea-level rise, famine due to agricultural losses, air pollution exposure from severe wildfires, displacement from homes and forced migration. The cumulative effects directly impact our environment, but also significantly impact our health and the collective health of our communities.
Similar to the broad and diverse impacts on our environment, climate change effects on human health are diverse - exacerbating existing chronic cardiopulmonary conditions, increasing inflammatory conditions and autoimmune diseases, and causing new health risks such as infectious disease outbreaks and novel heat-related diseases. Importantly, these effects are already happening, and despite efforts to slow or reverse climate change, elevated health risks will worsen and persist.
Efforts are underway to define climate and health impacts and mitigate their effects, however, these efforts remain nascent and insufficient to meet public health needs. Furthermore, the health effects of climate change are not evenly distributed and are intertwined with social determinants of health (SDOH), exacerbating health equity concerns and further threatening the most at-risk in our communities. At-risk populations, particularly in low-income and developing regions, face the greatest threats as they often have poor baseline health, compounded by SDOH, and lack the resources and infrastructure to adapt.
These combined health challenges, if not addressed, will continue to exacerbate this ongoing public health crisis. Solutions require an “all hands-on deck” approach involving academic institutions, researchers, health providers, community leaders, and policy makers. As a world-renowned university and health system, Duke University and the School of Medicine must help meet this climate and health challenge and lead efforts to improve the health of our communities by addressing the impacts of climate change on health.
Duke University and the School of Medicine (SOM) are uniquely positioned to be key thought leaders on human health impacts of climate change. Duke’s unique potential arises from the broad expertise of its faculty and staff, its world-renowned institutions (e.g. the Duke Global Health Institute, the Nicholas School of the Environment, the Duke Human Vaccines Institute, Duke Basic Science and Clinical Departments, other disease-focused Centers and Institutes, and the Margolis Institute of Public Policy), and a history of mobilizing to address critical human health challenges (e.g. work developing an HIV vaccine).
Duke also has a strong track record of collaborative science across the translational spectrum from basic discovery to implementation of therapies that advance health and improve community wellbeing. Duke’s commitment to translating research into practical solutions is particularly critical for climate and health concerns, ensuring that Duke’s Climate and Health discovery research will be focused on improving public health and informing health policies both locally and globally.
Duke can be highly impactful in addressing local and global Climate and Health concerns due to its active engagement in communities significantly impacted by climate change and its well-established international, national, and local partnerships with academic institutions and health centers. As Climate and Health is an unprecedented, multidisciplinary global challenge, requiring practical solutions to critical global health threats, Duke University, the SOM, and its local and global partners are uniquely positioned to meet this challenge.
To fully realize the Duke’s potential and have maximum impact on Climate and Health, we will need to engage faculty, foster new collaborative research teams organized, and develop even deeper connections with our communities and international partners. The potential is tremendous, but the effort required to reach this goal will be significant. This is a seminal moment where Duke can seize the opportunity to be a leading voice in the global public health crisis arising from climate change, allowing Duke to do what it does best - take on critical challenges in human health.
In recognition of the significance of climate change, Duke University launched its Climate Commitment in September 2022, establishing the Office of Climate and Sustainability. The Duke Climate Commitment focuses on five pillars: Education, Research, Sustainable Operations, External Engagement and Community Partnerships. Within the Climate Commitment Research pillar, Climate and Health was not, initially, prioritized. This reflects the complexity of the impacts of changing climate on human health and a need to define Duke’s potential to perform impactful research in this domain. Recognizing that gap, the SOM, in cooperation with the Duke Office of Climate and Sustainability, began in early 2024 to identify existing areas of Duke’s research strengths in Climate and Health. This effort has focused on identifying Climate and Health research domains where Duke could leverage its existing expertise, both in areas of ongoing Duke Climate and Health research, and where Duke could address new areas of research on Climate and Health. This landscape assessment has informed the proposed strategic framework to focus future Climate and Health research efforts.
The effort to describe Duke’s Climate and Health research landscape and outline areas where Duke can have the greatest impact has taken a bottom-up approach. This included over 60 meetings with key individuals and groups including Center and Institute Directors, Department and Administrative leaders, community groups, and individual faculty members (See Appendix A). In addition, the SOM faculty, associated Center/Institute faculty, and students (including medical students, graduate students and post-doctoral fellows) were surveyed. The focus of the survey was to learn about current Climate and Health research activities, define faculty and student interest in expanding into Climate and Health research, and to gather data to estimate of the level of support needed to initiate new Climate and Health research activities (Appendix G). Additional informational meetings occurred with the AME Zion HEAL Partnership, Duke Office of Community Health, and Resilient American Communities to gain an understanding of community perspectives on Climate and Health impacts and the extent of community-level concern. A separate second survey was administered to national Clinical Translational Science Awardees to gain insights on potential areas for future collaboration with other institutions and identify research areas where Duke could provide leadership. Finally, a landscape survey of federal and philanthropic institutions and foundations was conducted to identify areas of potential funding and interest in Climate and Health (Appendix H). An external panel of individuals and leaders from across the SOM and the University was convened (Appendix B) to review the accumulated data, develop thematic areas for proposed Climate and Health research, and suggest an operational structure under which this research could be directed and accelerated. Figure 1 summarizes the major points.
The Climate and Health Strategic Plan proposes the Duke Climate and Health Research Initiative (CHeRI). CHeRI is envisioned as an interdisciplinary, virtual initiative that will become a central hub for Climate and Health research and translational activities. It will serve as a convening hub for networking, non-formal learning, and grant-writing Climate and Health efforts, at Duke University. CHeRI will foster impactful Climate and Health research that is community-engaged and leverages Duke faculty and student expertise across the translational research spectrum.
As the organizing node for Climate and Health research, CHeRI will facilitate campus-wide faculty interactions and provide pilot grant support to multi-disciplinary programs that address critical Climate and Health concerns. Its guiding organizational principle would be a “OneDuke approach” (highlighted in Appendix C). CHeRI will partner with other campus Climate-related initiatives (e.g. the Climate Justice Center in the Sanford School of Policy, and the Climate Change and Global Health Initiative in the Duke Global Health Institute) to ensure efforts are wholistic, collaborative and support the mission of the Duke University Climate Commitment. CHeRI will also support collaborations with external partners, including existing Duke international (i.e. Duke NUS and Duke Kunshan), national (i.e. New York Climate Exchange), and local partners (i.e. North Carolina Environmental Justice Network, North Carolina Climate Justice Collective, Triangle Institute for Evolutionary Medicine).
Differentiators for the CHeRI and Duke’s Climate and Health research agenda:
- CHeRI, as a convening platform, will leverage existing Duke research strengths to develop innovative research and amplify impacts aimed at the intersection of Climate and Health.
- Initiatives will be informed by bi-directional partnerships with local and global communities.
- Research to impact will be prioritized by embracing, promoting, and connecting science across the translational spectrum. Through the integration of basic and population scientists, clinical investigators, and clinicians, Duke will accelerate basic discoveries using epidemiological, biostatistical, and implementation science methods, translate findings into new interventions in health, and inform global, national, and local policies.
- By developing a Climate and Health research portfolio, CHeRI will help develop and retain leading investigators with expertise in cross-cutting Climate and Health research areas and promote a culture of collaboration that nurtures investigators, providing the support needed to accelerate outstanding careers in science. The collaborative culture and research-to-impact agenda will attract new talent at all levels, including postdocs and medical students.
- CHeRI will be a nidus for engagement with other institutions, foundations and governmental agencies to advance Climate and Health research at Duke and foster collaborative research proposals.
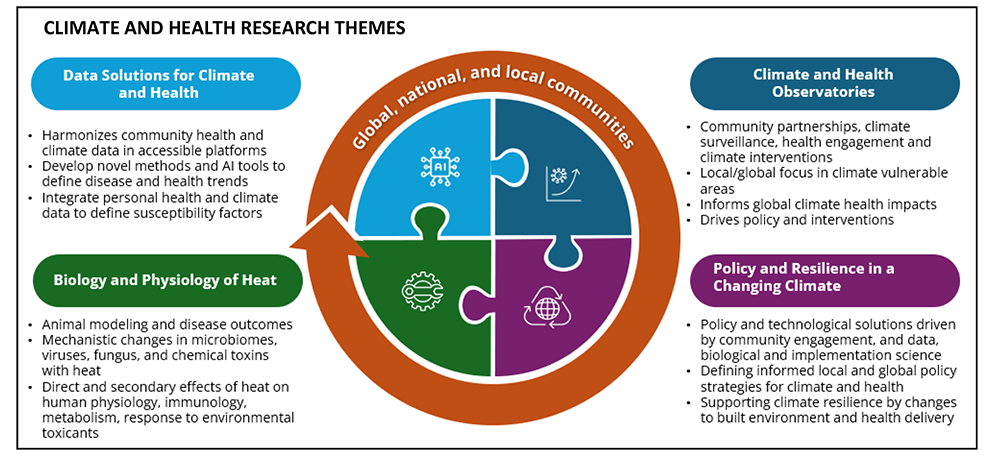
CHeRI would have four main themes under which Climate and Heath research will be organized and supported (Figure 2, expanded version Appendix D). Each theme covers a unique but interconnected topic area important to Climate and Health. CHeRI follows a discovery-to-impact facilitation approach where basic science defines the problem, translational science links this to interventions, implementation science measures the effects of interventions and informs policy strategies to mitigate harm to human health.
The themes are outlined below, including an example of a potential topic that could lead to impactful Climate and Health research. Appendix E outlines how the themes could be operationalized and provides additional examples of active and/or potential research that could be developed.
Theme 1: Biology and Physiology of Heat
As a major driver of climate change impacts, there is a critical need to define the myriad effects of heat on human health, including direct effects on human physiology and disease but also indirect effects such as how heat alters microbiomes, microbial pathogens (i.e. fungi and viruses), and chemical toxins, and how these heat-mediated alterations drive adverse human health effects. Determining direct heat impacts requires basic discovery science not only to define how heat impacts overall human physiology but also to identify the individuals/groups at most risk for severe health effects from heat (e.g. pregnant mothers, children, and the elderly). Possible immediate impacts include the potential for heat-modified host factors such as immune responses, vaccine effectiveness, cellular metabolism, cardiorespiratory functions, mental health and responses to environmental toxicants. These can be augmented by downstream climate change impacts such as increased agricultural losses from drought or heavy rain events, leading to bouts of malnutrition. Fluctuating access to nutrition is similar to the food insecurity experienced in communities that require government nutritional assistance, where periods of high nutrition (typically a calorically dense diet) are followed by malnutrition. In a positive feedback loop, this has the potential to significantly affect cell metabolism and metabolic disease incidence. An important research question is whether prolonged extreme heat exposure in the setting of food insecurity makes individuals more susceptible to development of later-in-life disease phenotypes.
Theme 2: Climate and Health Observatories
The effects of our changing climate are experienced across the globe including in areas of active Duke clinical and research activities in North Carolina, the Amazon River basin, East Africa and Southeast Asia. Duke’s presence in these locations offers a unique opportunity to engage in community-driven research into issues that are foremost in each location, to measure general and region-specific Climate and Health effects, and to drive policy and built environment and infrastructure strategies (e.g. creating resilient health systems and community-designed climate action plans) to mitigate health effects. For example, changes and shifts in seasonal temperatures, precipitation patterns, and the increased frequency of extreme weather are impacting the emergence and spread of vector-borne diseases. Observatories will accelerate the development of critical surveillance strategies, technologies, and models to describe and measure how climate change is altering the range of vector-borne diseases and develop, in close community partnership, effective interventions and public health strategies to mitigate effects. Importantly, learning about effective interventions in one location may inform interventions elsewhere, facilitating a global exchange of information and best practices.
Theme 3: Data Solutions for Climate and Health
Extreme weather due to climate change has already led to the development of a new disease, Chronic Kidney Disease of unknown origin, and has the potential to lead to more, while also increasing the incidence and worsening of known diseases (i.e. asthma, type 2 diabetes, coronary artery disease). At present, there is limited understanding of the specific impacts of climate change on disease development and exacerbation and limited methods to prospectively surveil at-risk communities. Addressing these gaps will require novel data and novel methods of data collection. Well-curated climate data needs to be linked to social determinants of health and health data and made available to Duke researchers and community organizations (such as public health organizations, local and county governmental entities, and health advocacy groups) to accelerate research and local and international collaborations to define climate impacts on health and drive solutions. These data are needed at an individual and aggregated level to allow investigators to identify trends, establish causal associations, and predict future events. A central data repository and infrastructure is needed to collate, curate and share these data with researchers, community members, and the health system to advance climate research. Novel epidemiological and biostatistical methods, AI algorithms, and predictive modeling will be required to design studies and analyze vast amounts of data to forecast disease spread, identify of high-risk populations, and thereby develop targeted interventions to mitigate risk.
As an example of how a data platform could benefit our immediate community, consider the potential for improving the health of Duke Health patients by incorporating risk of heat related complications into their preventive health and treatment strategies. Duke Health does not presently collect data on the effects of extreme and prolonged heat events on its patients and there is no information on the optimal approaches to quantify heat, diseases impacted by heat, associated heat infections and exposures (e.g. waterborne illnesses and environmental toxins) and the individuals most at risk. Furthermore, it is not clear how heat leads to acute health visits, the care reforms required to prevent heat-related complications and the associated impacts to health system preparedness for these events. Leveraging AI efforts underway in Duke Health with climate data and predictive modeling could define and predict risk and develop intervention strategies (e.g. personalized MyChart alerts and interventions for heat) that could improve the health of Duke Health patients.
Theme 4: Policy and Resilience in a Changing Climate
Key to responding to Climate and Heath threats is a combination of interventions that promote community resilience and policy measures supporting these efforts. New policies to build resilience in communities, institutions, and health systems will be crucial to enhancing adaptive capacities, reducing vulnerabilities, and promoting sustainable development in the face of climate-related challenges.
As an example, research performed at Duke suggests that nighttime, and not daytime, temperatures are associated with worsened maternal health outcomes. However, most public health policies are directed at making daytime cooling centers available during peak temperatures. Effectiveness and implementation trials could measure maternal health outcomes associated with different strategies to provide nighttime cooling interventions which could then inform health policy changes. As another example, while North Carolina is implementing Medicaid coverage expansion and payment reforms across all public programs intended to reduce health disparities and address unmet social needs, the Duke Margolis Institute for Health Policy identified these major policy reforms do not yet account for any adjustments that may be needed to address increased risks of climate-related extreme health events and exposures, representing an important Climate and Health policy concern.
To operationalize the proposed Climate and Health strategic plan, CHeRI will require a combination of Duke institutional and philanthropic and external funder support. Initial support will require internal financial commitments, but this investment will be amplified through successful grant applications to philanthropic, federal and international sources. Specific suggested infrastructure needs will include administrative infrastructure, symposium and networking events, funding for startup and existing research activities, community engagement, recruitment and funding for faculty and trainees.
For more information contact: SOM_climatehealth@duke.edu