Researchers at Duke University School of Medicine have found that tapping into the nervous system could help reduce the gut inflammation that drives inflammatory bowel disease (IBD).
A new study led by Luis Ulloa, PhD, and Wei Yang, PhD, reveals how electrical stimulation of the vagus nerve—a major nerve connecting the brain and gut—may combat the stress-related inflammation that worsens IBD symptoms.
The findings published in Science Translational Medicine offer new insights on the brain's role in gut health.
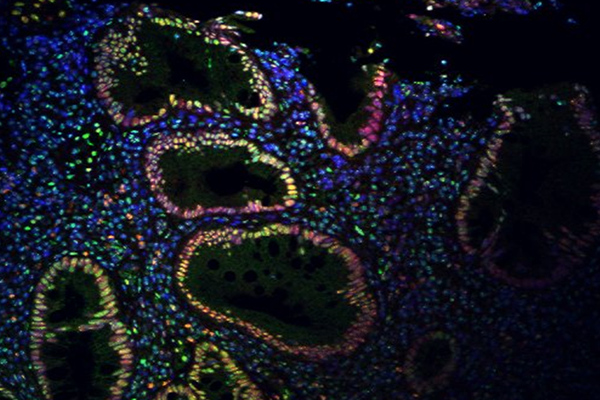
Duke researchers showed vagus nerve stimulation in stressed mice with colitis, a form of IBD, significantly reduced inflammation, alleviated symptoms, and improved survival rates. By engaging the parasympathetic nervous system, the team observed that inflammation could be eased by controlling SUMOylation, a cellular process that shapes immune response.
Modulating SUMOylation—either through vagal nerve stimulation or treatment with a SUMOylation inhibitor—could open the door to IBD therapies that focus on managing inflammation directly, rather than alleviating symptoms.
In 2022, Duke researchers, backed by the National Institutes of Health, began investigating whether stimulating the vagus nerve could affect SUMOylation and set off a natural anti-inflammatory response that calms immune responses and reduces inflammation.
The new study is the first to show that targeting specific forms of SUMOylation could prevent the harmful influx of immune cells that can trigger gut inflammation. First study author and former Duke research scholar Ayman Youssef, MD, a clinical fellow of autonomics at Vanderbilt Medical Center, analyzed data identifying that inhibiting SUMOylation, through genetic or drug-based approaches, dramatically slowed disease progression in mouse models.
“One surprising finding of this study is that inhibiting SUMOylation appears to mimic the beneficial effects of vagal stimulation, resulting in improved clinical symptoms of colitis,” said Yang, professor of anesthesiology and associate professor of neurology at Duke School of Medicine.
IBD cases are soaring—up 50% in the last 15 years. Scientists are intensifying efforts to reduce inflammation-causing cells in the intestines and improve treatment options for the nearly 7 million people affected worldwide.
IBD includes two primary types: ulcerative colitis, which affects the colon, and Crohn’s disease, which can inflame any part of the digestive tract. Both conditions disrupt lives and can lead to serious complications like colon perforation, cancer, and even early death.
Current anti-inflammatory treatments bring relief but often fall short, as patients can stop responding to medications over time, suffer relapses, and experience significant side effects.
Researchers have long noted that stress plays a significant role in exacerbating IBD symptoms, and some have even described ulcerative colitis as psychosomatic.
“Stimulating the vagus nerve neutralized the effects of stress and restored a balanced and healthy physiologic state,” said Ulloa, a Duke anesthesiology researcher and corresponding author of the study. “Many relaxation techniques, like deep breathing and meditation, are designed to enhance the parasympathetic system, with the vagus nerve playing a central role in relaxing most of our organs.
“Although previous studies have suggested the role of the vagus nerve, our study demonstrates that its effect is mediated through regulating SUMOylation,” he said.
Ulloa warns that not all patients may respond similarly, and translating the findings from lab studies to clinical settings could lead to varying outcomes, or no benefit at all. The approach, called “bioelectronic medicine,” is part of an emerging field where nerve stimulation is being explored to treat various inflammatory conditions from rheumatoid arthritis to Crohn’s disease.
Additional Authors: Ata Ur Rehman, Mohamed Elebasy, Jatin Roper of Duke School of Medicine; Shehzad Z. Sheikh of University of North at Carolina Chapel Hill and Jorn Karhausen, of Duke and Humanitas Research Hospital.
Funding for the study was provided by the NIH National Center for Complementary and Integrative Health (AT011387), National Institute of Diabetes, Digestive and Kidney Diseases (P01DK094779, 1R01DK104828, and P30-DK034987) and the Helmsley Charitable Trust.