Over the past 40 years, HIV research has done more than transform a once-fatal infection into a manageable chronic disease — it has revolutionized entire fields of medicine.
In a new paper published in Nature Medicine, investigators including those from Duke Global Health Institute, conclude that decades of sustained U.S. investment, collaboration between academia, industry, and government, and the urgency of a global health crisis led to breakthroughs that now underpin treatments for cancer, tuberculosis, hepatitis, and even COVID-19.
Here are ten major advances that owe their roots to HIV research and the ongoing fight for a protective vaccine — proof that bold, continued investment in discovery doesn’t just save lives, it drives all of modern medicine forward.
1. Turning HIV into a manageable condition
An HIV diagnosis in the 1980s was considered a death sentence. Today, thanks to combination antiretroviral therapy (ART), most people with HIV can expect a near-normal lifespan. ART not only suppresses the virus but also prevents transmission — and related discoveries, like pre-exposure prophylaxis (PrEP), now make HIV infection entirely preventable. These are among the most impactful medical advances of our time.

2. Building the foundation of modern immunology
To understand HIV, scientists had to map the immune system in unprecedented detail — from how T cells and antibodies work to how viruses evade them. That effort built much of today’s modern immunology, deepening our understanding of the innate and adaptive immune responses that protect us from all infections, not just HIV.
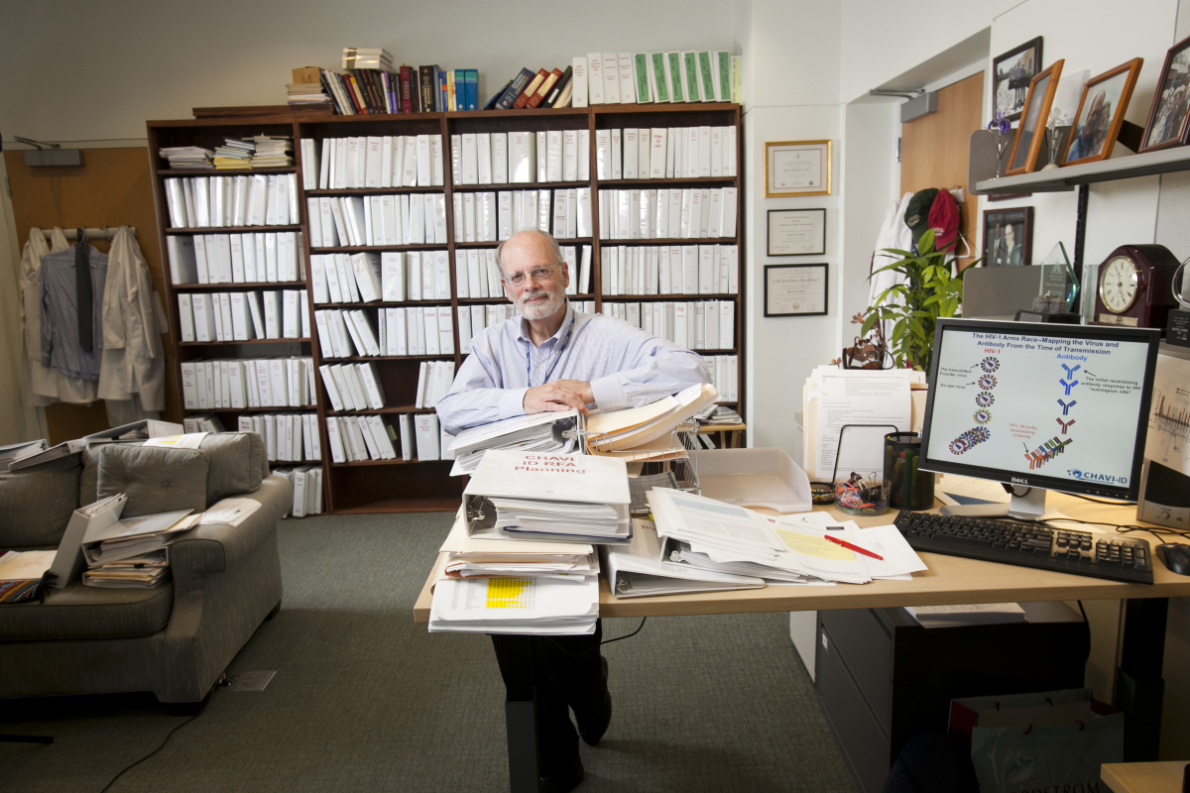
Notably, at the forefront of this work was Barton Haynes, MD, director of the Duke Human Vaccine Institute (DHVI). Haynes and the DHVI pioneered studies on broadly neutralizing antibodies and the mechanisms of immune evasion, laying the groundwork for strategies that now guide vaccine development against HIV and other pathogens. These contributions were instrumental in shaping the modern understanding of how to harness immunity for prevention and treatment.
3. Redefining tuberculosis treatment
Because HIV and tuberculosis (TB) often occur together, HIV studies transformed how we diagnose and treat TB — the world’s deadliest infectious disease. NIH-funded research shortened TB treatment from six months to four, developed a one-month preventive therapy, and led to new drugs for resistant strains. These discoveries now shape TB care globally.
4. Advancing hepatitis B and C treatment
Several of today’s leading hepatitis drugs — like lamivudine and tenofovir — were first developed for HIV. In addition, the “test and treat” model used to prevent HIV transmission inspired global campaigns to identify and treat hepatitis B and C infections.
5. Powering cancer immunotherapy
The same science that tried — and initially failed — to use T cells to fight HIV paved the way for modern cancer immunotherapies. Techniques such as CAR-T cell therapy and immune checkpoint inhibitors emerged from HIV research into how to manipulate immune cells. The lessons learned in HIV now help train the immune system to destroy tumors. Many forms of fatal cancer have become treatable with immunotherapies.
6. Preparing the world for a pandemic
The rapid creation of COVID-19 vaccines didn’t come out of nowhere — it came from the HIV research ecosystem. The vaccine platforms, monoclonal antibody technologies, and clinical trial networks that powered Operation Warp Speed were built on decades of HIV science. Even Paxlovid, the oral antiviral, uses an HIV-derived drug booster (ritonavir) to increase its effectiveness.
Duke researchers in DHVI put these capabilities in place, by finding broadly protective antibodies to early COVID strains, developing COVID vaccine immunogens, manufacturing vaccines, and leading clinical trials.
7. Illuminating the biology of aging
People living with HIV often experience accelerated aging — developing conditions like heart disease and osteoporosis earlier. Studying these patterns has given scientists a living model for understanding aging itself. Trials such as the REPRIEVE study, which showed statins can prevent heart disease in people with HIV, are now shaping cardiovascular prevention for everyone.
8. Revolutionizing public health and care models
HIV care reimagined medicine as a team effort. Clinics like San Francisco General’s Ward 86 pioneered “one-stop” models that combined medical, psychological, and social services — now standard in chronic disease management. Community advisory boards, integrated research within primary care, and global “test and treat” strategies all began in HIV medicine.
9. Accelerating gene and vaccine technologies
Efforts to create an HIV vaccine — and a potential cure — have driven major progress in gene editing, viral vector design, and antibody engineering. Even if a one-time HIV cure remains elusive, these technologies are already powering new vaccines for other infections and innovative treatments for autoimmune diseases and cancers.
Over the past two decades, Haynes at Duke has led three major NIH-funded programs that have mapped how HIV attacks the body, uncovered why it’s so hard to stop, and designed new vaccine strategies to trigger powerful immune defenses.
10. Showing how science builds on science
The story of HIV research is a story of ripple effects. From immunology to geriatrics, oncology to pandemic response, each investment in HIV discovery has fueled broader innovation. Continued U.S. leadership in HIV science doesn’t just safeguard progress against the virus — it underwrites the future of global health itself.
Bottom line:
HIV research changed the course of medicine — not just for those living with HIV, but for all of us. The breakthroughs born from this field remind us why sustained, curiosity-driven research remains one of the most powerful tools for improving human health and advancing scientific leadership.