
Sound Action
What does the rustle of tall grass mean to you? If you live in northwest Alaska, it could well mean your livelihood.
A hundred miles from Russia along the shores of the Bering Sea, the remote region is home to three cultural groups—the Inupiaq, Yup’ik and Siberian Yupik—that depend on hunting, whaling and fishing for survival. The ability to discern that rustle, a ripple, the call of a bird, is essential.
But these communities, like so many rural low-income communities worldwide, are disproportionately affected by hearing loss. An estimated 500 million people experience disabling hearing loss—a number expected to exceed 900 million by 2050—and more than 80 percent of affected individuals live in low- and middle-income countries. And while Alaska is in a high-income country, a child there is strikingly five to six times more likely to experience hearing loss than among children in the general U.S. population.
Genetics, nutrition and access to health care are likely contributing factors. But there’s much yet to learn.
“Those are really staggering statistics,” says Susan Emmett, an assistant professor of surgery and global health at Duke. “It means that there is a lot of work to be done.”
Emmett’s mission is to stop preventable hearing loss in Alaska and beyond. For the past few years, she has been working with Nome, Alaska-based Norton Sound Health Corporation to improve school-based hearing screening. The study, called the Hearing Norton Sound project, focuses on 15 communities ranging in size from 100 to 1,000 residents. Some are on islands in the Bering Sea, and all are reachable only by helicopter or bush plane. None has resident doctors or nurses.
Hearing-loss evaluation customarily requires an in-office visit with an audiologist and, often, an ear, nose and throat surgeon, which usually would reuare rural Alaskans to make expensive and complicated trips to larger medical facilities. Instead, Emmett and her collaborators are leveraging Alaska’s robust telemedicine technology to improve the school hearing screening and referral process.
In the study, community health aides, who provide the vast majority of health care in the region, connect with audiologists and surgeons via telemedicine to collect data on children with suspected hearing issues identified during school hearing screenings. The aides send high-resolution digital images of the ear and other test results, enabling specialists to diagnose problems remotely.
In a state in which 75 percent of communities aren’t connected to a hospital by road, this means considerable savings in time and money, and far more children receiving a timely diagnosis and therefore appropriate care and a chance for improved health outcomes. The World Health Organization estimates that half of all global hearing loss can be prevented.
“Our colleagues in Alaska have validated that telemedicine consultation is equivalent to an in-person exam,” Emmett says. “The same decisions are being made for patient care.”
To date, she says, telemedicine in Alaska has been used solely for clinical care. “We’re applying telemedicine with a paradigm shift. We’re applying it for prevention.”
Losing More than Hearing
The smallest of the communities in the study is the island of Little Diomende. “When we go there, we travel by helicopter,” says Samantha Kleindienst Robler, Norton Sound Health Corporation’s director of audiology and co-principal investigator of the project. “If the winter is cold enough, the ice will sometimes freeze thick enough to allow a plane to land,” though she can’t recall when that last occurred.
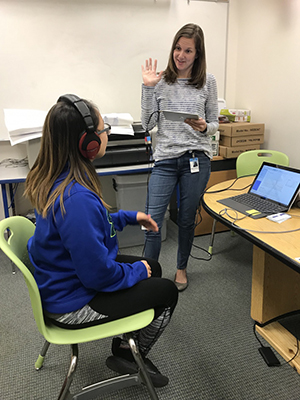
Health Corporation’s director of audiology
and co-principal investigator of the project,
conducts a hearing evaluation with a child.
These communities nurture an oral tradition. Storytelling—along with carving, beadwork, dancing and drumming—lies at their cultural core. Hearing loss, Robler observes, can lead to isolation, particularly among elders, and deterioration of many critical aspects of culture.
“There are multiple consequences beyond the sensory impairment,” says Blake Wilson, co-director of the Duke Hearing Center and DGHI affiliate, who has been a champion for recognition of hearing loss as a global health concern. In addition to social isolation, he cites limited job opportunities for those with impaired hearing. “From a global and national perspective, hearing loss impedes economic growth.”
“There are also highly significant associations between hearing loss and various deleterious health conditions, including dementia,” he says.
Earlier this year, Wilson, a pioneer in the development of signal-processing strategies for cochlear implants, was named to lead a Lancet Commission to address the global burden of hearing loss.
Emmett and Debara Tucci, a Duke professor of surgery and DGHI affiliate, will be members.
“Hearing loss is definitely under-recognized as a global health issue with expansive implications for health and economics, but there’s a lot of momentum right now, and I believe that’s changing,” Emmett says. “We have really good evidence to show that the impact of hearing loss is profound and lifelong.”
The next big step, she says, is drawing awareness to those lasting implications, “and we’re starting to make strides in that regard.” The World Health Assembly, the decision-making body of the World Health Organization, passed a resolution on hearing loss in 2017 that she and her colleagues had been pushing for several years.
“Dream Big"
Emmett’s interest in global hearing loss traces to more than a decade ago, when she arrived at Duke as a medical student with a strong interest in health policy.
“That interest became more international in nature as I advanced in medical school,” she says. “I really wanted a chance to live and work abroad in low-resource settings, because I don’t feel you can commit to a career in global health until you’ve experienced what it means to do field research and live in that type of environment.”
Emmett spent her third year of medical school conducting pediatric HIV research in Tanzania through a Howard Hughes Medical Institute Research Training Fellowship. In the course of that work, she was struck by the prevalence of unattended hearing loss. It sparked a recognition of hearing loss as a neglected area of public health.
“Ultimately,” she says, “my clinical interests aligned with this interest. I really enjoyed otolaryngology, and ear surgery in particular, but I also knew I wanted a global health research career. That time in Tanzania was transformative because it helped me see that I could bring these two things together.”
Emmett did a seven-year otolaryngology residency at Johns Hopkins University, where she also earned a master’s degree and did a postdoctoral fellowship, both in public health. She then returned to Duke to join the faculty. In 2017, she was selected to the TED Fellows program in recognition of her contributions to hearing-loss prevention. To date, she is the only Duke physician whose TED talk was published on TED.com.
“I think she’s spectacular,” Blake Wilson says of his colleague, “and that view is shared by many. She’s already a superstar at a relatively young age, and her research is outstanding and multifaceted.”
“My goal is to reduce hearing-loss disparities globally,” Emmett says, “and the work in Alaska is absolutely essential to that because it’s working on diagnosis—specifically, how we improve access to care in remote populations.
“But that’s not the only piece to the puzzle.” Last fall, she launched the Global HEAR Collaborative, the first-ever international hearing-loss evaluation, advocacy and research network, with members from 22 countries. “The goal, and the ultimate rationale, is that by working together across countries we can answer questions about hearing loss that are impossible to answer working alone.”
“We’ve all come together to build this network,” Emmett affirms, “that will help us go to the next level, to start answering larger questions about hearing loss, how we change access to care and how we stop preventable hearing loss from ever occurring.
“You have to dream big.”
Taylor Sisk is a Nashville, Tennessee-based health care journalist covering Appalachia and the southeast.
This story first appeared on the Duke Global Health Institute website.
