
A Personal Fight, A Precision Approach
Ron Klarin’s cancer journey began in Florida with a CT scan that revealed a small lung nodule—one his doctors initially dismissed as low-risk. “They told me it was probably nothing. There was no urgency,” he said.
At the time, Klarin and his wife Bonnie were preparing to move to North Carolina to be closer to family. After the move, his symptoms escalated, including severe coughing with any physical activity. A PET scan and biopsy at a local hospital revealed small cell lung cancer that had already spread to his bones and lymph nodes.
Initial rounds of chemotherapy were rough, leading to hospitalizations. “After the first infusion, I was in the hospital for a week with sepsis. The second time, it was pneumonia and six days with chest tubes.” Seeking a more coordinated approach, Klarin turned to Duke Health.
At Duke, further imaging brought the unexpected news of two metastases in his brain. “That was a blow. I was devastated,” Klarin said.
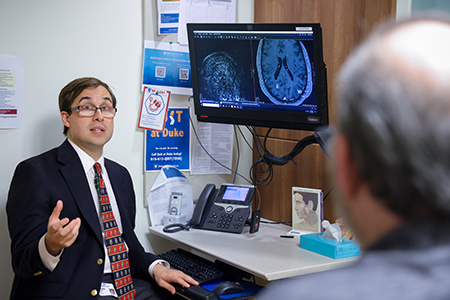
Soon after he met radiation oncologist Eugene Vaios, MD, MBA, a member of the Duke Cancer Institute, an assistant professor in the Duke Department of Radiation Oncology and member of the Duke Center for Brain and Spine Metastasis (DCBSM).
“But meeting Dr. Vaios really changed my outlook. He put me so far at ease that I went from a state of high anxiety to, ‘Okay. Let’s do it.’”
Vaios recommended stereotactic radiosurgery (SRS), a focused, high-dose radiation technique that targets tumors while sparing healthy tissue and reducing side effects.
“Dr. Vaios was extremely thorough,” Klarin said. “We went through the scans multiple times, and he explained everything in a way that made sense. That kind of attention builds trust.”
SRS treatments made a measurable difference. “The metastases in my brain have basically been eliminated,” said Klarin, who continues his care at Duke. “There’s still some inflammation and necrosis, but it’s trending in the right direction.
“Small cell lung cancer isn’t easy to treat, but I’m confident in the outcome of my treatment,” he said. “The care you experience, especially as a cancer patient – it really makes a difference where you go for treatment, and I’ve been so impressed with the quality of care I’ve received here.”
Precision Approach to a Complex Challenge
Since its launch in 2017, Duke Center for Brain and Spine Metastasis has grown into one of the most comprehensive programs of its kind, treating patients whose cancer has spread to the brain, spine, and other parts of the central nervous system.
Radiation oncology plays a central role, delivering targeted stereotactic radiosurgery (SRS) for hard-to-treat tumors.
“We’ve been doing radiosurgery at Duke as a collaboration between neurosurgery and radiation oncology in earnest since the early 2000s,” said John Kirkpatrick, MD, PhD, professor of radiation oncology and neurosurgery and director of radiation oncology for the DCBSM. “But with the formation of DCBSM, we’ve made the multidisciplinary secret sauce: adding palliative care and a strong medical oncology component to neurosurgery and radiation oncology.”
SRS has since become a cornerstone of care, used not just for brain metastases but for recurrent gliomas, acoustic neuromas, meningiomas, and arteriovenous malformations. Over the last 20 years, Duke has treated more than 5,000 patients with SRS and stereotactic body radiation therapy (SBRT).
That record is backed by a team known for precision and empathy. “I’m proud to work with a team that places top-level patient care first,” said Scott Floyd, MD, PhD, deputy director for research.

What Sets Duke Apart
DCBSM’s model of care centers on rapid access and team-based navigation. Every patient referred to the Center is guaranteed an appointment within 72 hours with a team of specialists, all in one place, on the same day. Each patient is also matched with a navigator to streamline testing and appointments.
“The treatment of brain and spine metastases is complex,” said Trey Mullikin, MD, radiation oncology deputy director for spine metastases. “What makes our Center unique is how quickly we coordinate across specialties.”
Supporting the clinical side is a group of expert radiation physicists, who guide treatment planning, imaging, and delivery. Their work goes beyond the clinic, said Chunhao Wang, PhD.
“Our physicists also lead research in advanced imaging and AI to make treatments more consistent and better monitor outcomes,” he said.
Palliative care became a part of the team’s approach in 2018 to support patients with serious illnesses and complex treatment plans.
“The collaboration between palliative care and the DCBSM has been invaluable,” said Betsy Fricklas, PA-C. MMSc, palliative care director. “It allows us to offer a holistic approach that prioritizes not only disease treatment but also symptom management and emotional well-being.”
Rewriting the Rules on Research Access
Historically, patients with brain or spine metastases were excluded from clinical trials. Duke is changing that. DCBSM trials focus on personalized approaches—from advanced imaging that tracks spinal tumors to novel therapies guided by real-time imaging.

Research is fueling progress. Over the past decade, DCBSM researchers have earned grants to develop brain tissue-based treatments, refine pediatric radiation strategies, and studying tumor DNA as a non-invasive biomarker for glioblastoma.
“Looking forward, the really exciting part of the Center is that the research work we are doing will lead to even better results for our patients,” Floyd said.
Recent findings are changing care far beyond Durham. Duke researchers led the largest single-institution study combining SRS with immunotherapy and were the first to report long-term outcomes with dual immune-checkpoint inhibitors in brain metastases from melanoma or lung cancer. The results showed that this combination significantly improved tumor control in the brain.
But timing matters. A follow-up study showed patients receiving checkpoint inhibitors within four weeks of SRS faced a higher risk of radiation necrosis—swelling and damage to healthy brain tissue. These findings, based on data from 288 Duke patients, are helping doctors nationwide fine-tune how they deliver care.
As the Center pushes the frontier of cancer treatment, philanthropy remains a driving force, including support from the Klarins who began donating in 2024.
“The support from federal, foundational, and philanthropic funding sources is critical to our mission of improving patient care for patients with brain and spine tumors,” said Duke radiation oncologist Zachary Reitman, MD, PhD.
Sarah Brady is assistant director of Communications and Marketing for the Department of Obstetrics and Gynecology and the Department of Radiation Oncology.
Photos by Huth Photography.
