How Biomedical Innovation is Transforming Stroke Recovery
Biomedical engineering is rapidly reshaping and revolutionizing stroke care. At the forefront of this transformation is Wayne Feng, MD, professor of neurology and biomedical engineering, director of the Duke Comprehensive Stroke Center, and chief of the Stroke and Vascular Neurology Division.
Since his arrival in 2019, he has led a team and built one of the nation’s top-quality clinical and research stroke programs. His Neuromodulation and Stroke Recovery Lab (NM-SRL) focuses on harnessing non-invasive brain stimulation tools as potential treatment options for post-stroke complications, including motor impairment, visual field deficits, and pain syndrome.
Strokes happen when blood flow to the brain is interrupted, usually by a clot or a ruptured blood vessel. The surrounding brain tissue becomes deprived of oxygen, leading to cell death and devastating effects on movement, language, and vision for stroke survivors.

Stroke remains one of the leading causes of death, and the leading cause of serious, long-term disability, for adults in the U.S. Time is the critical factor in immediate stroke care: if caught quickly enough — within about 4.5 hours of onset — patients can often receive a clot-busting medication before the stroke takes full effect. Unfortunately, only about 7-8% of stroke patients in the U.S receive treatment in time.
After a stroke, the stroke-affected side has less cortical excitability, while the unaffected side works overtime. Recovery after stroke requires modulating brain activity to retrain the brain and restore lost function.
Feng has pioneered several non-invasive methods to modulate brain activity. By activating the impaired hemisphere or reducing over-activity in the opposite hemisphere, these devices can correct imbalances in the brain, which can then induce behavior changes and better clinical outcomes.
“A brain modulation tool is capable of influencing the motor cortex excitability, either exciting or inhibiting,” Feng said. “To keep brain tissue alive after a stroke, we engage residual tissue and induce brain plasticity.”
Ultrasound: Breaking New Ground
One promising approach is low-intensity intensity focused ultrasound stimulation (LIFUS), which has been shown to both inhibit and excite the motor cortex in healthy individuals. Building on these findings, Feng and his team recently completed a first-in-human, Phase I intensity/dose escalation trial to determine the safety and feasibility of LIFUS in stroke patients.
“Acoustic intensities below the FDA safety limits for diagnostic ultrasounds is likely safe for stroke patients,” Feng said. “We have also recently explored the effect of LIFUS on motor learning and corticospinal excitability in the affected arm of stroke patients.”
After a 12-minute ultrasound session, participants were given a five-button keyboard and were asked to watch a computer screen with five boxes on it, each corresponding to one keyboard button. When a circle appeared in one of the boxes, participants were cued to hit the corresponding button using their stroke-affected hand.
The results, published in the journal Brain Stimulation — the leading neuromodulation publication — were very encouraging. Two-thirds of participants improved in motor sequence learning, which is the brain’s ability to relearn and refine movement sequences. Over 75% showed enhanced corticospinal excitability. The groups at higher intensity showed better effects. No participant experienced any adverse effects.
While still early, these findings suggest that LIFUS is not only safe but also a potentially effective way to enhance motor skill learning. A phase-II clinical study is in the works.
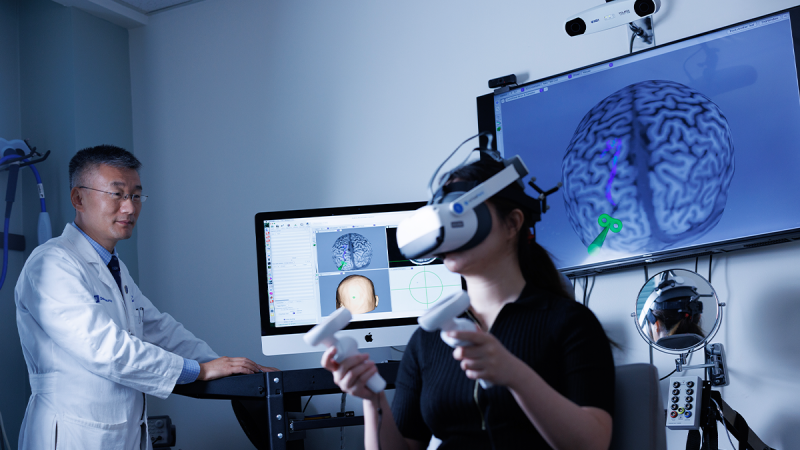
Vision Rehabilitation via Virtual Reality
LIFUS may also be useful when paired with virtual reality (VR). Visual impairments affect around 30% of stroke patients, with 16% experiencing permanent visual field deficits. Among other consequences, this robs many stroke patients of their ability to drive. Currently there are no strong evidence-based treatments for this type of visual field deficit.

Feng and his team are pioneering a combined LIFUS and immersive VR system to retrain the brain’s visual processing abilities. They are currently investigating if LIFUS can amplify the effects from VR.
VR can simulate real world activities, walking, maneuvering around obstacles, and playing game, helping patients to regain visual function. VR offers a treatment that can be done both in clinics at home for further practice.
“It is easy to use, can increase engagement and motivation, and offer the ability to practice functional tasks in a safe and controlled environment,” Feng said. “It can be tailored to individual needs, promote neuroplasticity, and potentially lead to faster and more effective recovery.”
FDA just made non-signficant risk determination for the study, and Feng is hopeful to begin clinical trials on this soon.
Neurostimulation at Home
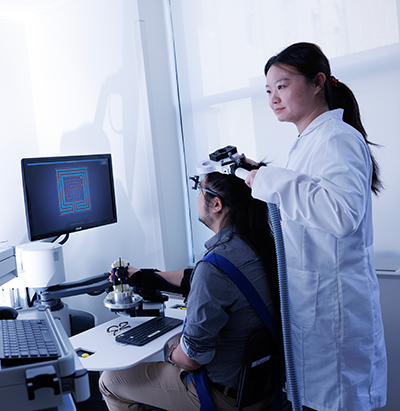
Repetitive transcranial magnetic stimulation (rTMS) is another noninvasive technique that uses a coil placed on the scalp to generate an electrical pulse from magnetic fields to stimulate brain cells to help prepare the patient for physical therapy.
Feng’s group is currently funded by the National Institutes of Health to conduct a two-center Phase II clinical trial to investigate the combined effect of rTMS and aerobic exercise compared to either approach by itself for stroke patients with both depression and walking deficits.

Another form of neurostimulation, transcranial direct current stimulation (tDCS), a technique Feng has devoted much of his career to translating, is a much smaller device that uses a very weak current powered by a 9-volt battery to excite brain cells. Compact and portable, it can clip onto the patient’s belt, allowing them to receive the treatment and physical therapy at the same time in a clinic or even at home.
“This device offers treatment that is easy to use, safe, and, most importantly, can be paired with rehabilitation therapy at the same time,” Feng said. “You can train the patients and their caregiver on how to use the device so they can use it at home without having to go to the clinic.”
In the last 5-plus years, despite challenges from the COVID-19 pandemic, Feng led a national consortium and completed a multi-center Phase II tDCS dosing selection study, published in Lancet Neurology May 2025. While the results were neutral, it highlights the need for further optimization of dosing protocol.
A More Personalized Future
These innovations are transforming what’s possible for stroke recovery — expanding treatment options and making therapy more accessible and effective for stroke patients, including those who are economically disadvantaged. The tools Feng is exploring offer hope for improving motor skills, restoring vision, and enhancing quality of life for millions of stroke survivors.
As research progresses into larger clinical trials, the future of stroke rehabilitation is poised to become more personalized, technology-driven, and empowering, offering patients and families new avenues for recovery and functional independence.
Alissa Kocer is a communications strategist in the Office of Strategic Communications at the Duke University School of Medicine.
Photography by Eamon Queeney, assistant director of multimedia in the Office Strategic Communications at the Duke University School of Medicine.