Someday, waiting lists for organ transplants will be a thing of the past.
“One day, patients will have access to regenerative medicine treatments that will circumvent the complications of organ donation,” says Sharlini Sankaran, PhD, executive director of Duke’s Regeneration Next Initiative. “We will be able to use our bodies’ own innate repair mechanisms to eliminate the wait time, cost, and limited supply of organ transplantation. Instead of transplanting organs, we will know how to repair our own.”
And this is just one of the possibilities of regenerative medicine, a field with historical reference in the myth of Prometheus and an exciting future unexpectedly linked to the remarkable regenerative capabilities of a small, striped freshwater fish, the zebrafish (Danio rerio). Regenerative medicine seeks to restore organ function without organ donation or transplantation. Instead, scientists attempt to either engineer or regenerate human cells, tissues, or organs—achievements that in the not-too-distant past were more likely to be found in science fiction than in working labs.
The Regeneration Next Initiative, established in 2016, is Duke University’s answer to how to best harness the potential of the rapidly expanding and innately interdisciplinary field. Regeneration Next strives to connect, support, and further the efforts of more than 60 faculty from across the School of Medicine, Pratt School of Engineering, and Trinity College of Arts and Sciences. Duke is the ideal place for this coalescing effort. “All the ingredients are coming together here, under one roof,” says Sankaran. “Our goal is to bring together the very best faculty and trainees doing this exciting work, and facilitate education, discovery, and the translation of research into treatments for patients.”
Several Duke biomedical engineers and scientists have already made startling discoveries in regenerative medicine. Ken Poss, PhD, director of Regeneration Next and the James B. Duke Professor of Cell Biology and professor in medicine, pioneered research on regeneration of cardiac muscle in zebrafish and hopes to identify the pathways in the human heart that could one day lead to similar regrowth of damaged tissue. With close to 70 percent genetic similarity and many of the same major organs and tissues as humans, zebrafish are ideal models for researchers to study the mechanisms underlying the regeneration of the heart, spinal cord, skin, joint tissue, and brain cells, in the hopes of unlocking similar latent processes in humans.
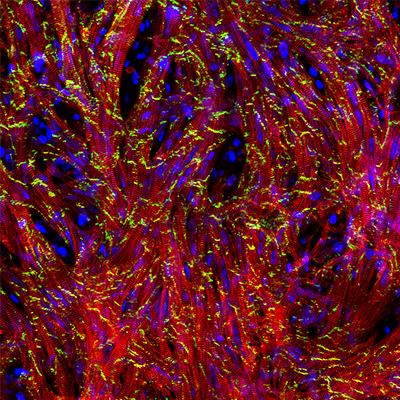
Nenad Bursac, PhD, co-director of Regeneration Next and professor of biomedical engineering, is taking a different approach but with a similar goal in mind: to change the way we treat the leading cause of death in the United States, heart disease. His team has bioengineered cardiac patches consisting of human heart muscle cells. Instead of losing function in an area damaged by a heart attack to scar tissue, an engineered cardiac patch placed over the affected area could one day restore the heart’s ability to fully contract and transmit electrical signals as healthy tissue does.
Complex challenges require multifaceted approaches. The current focus of Regeneration Next is on investing in individuals who are at the forefront of discovery research at various levels and across numerous fields. Attracting talent is a top priority; recent faculty appointments include Purushothama Rao Tata, PhD, assistant professor of cell biology, who researches cellular mechanisms of repair and regeneration in lung epithelial tissue. Supporting a collaborative environment among faculty and students from different departments and labs is another. Faculty-led informal gatherings, dubbed “Chalk Talks,” are held monthly for researchers to come together to share ideas and findings that have not yet been published. And Regeneration Next invests heavily in the careers of talented postdoctoral students through fellowships. “Postdoctoral researchers are at a very early point in their careers; they have fresh ideas and are willing to take risks,” says Sankaran. “They want to eventually establish their own labs and undertake risky work, and often this type of work can be difficult to fund.”
Regenerative medicine has the potential to radically change the treatment of injury and disease. There may be a day when patients suffering from paralysis regain movement, when a scarred heart reverses course through regeneration, and when a diagnosis of Alzheimer’s or Parkinson’s no longer means inevitable neurodegeneration. And, as lifespans increase, knee cartilage worn to the bone by decades of function, for example, might be repaired by injecting a regenerative trigger rather than surgical replacement, enhancing mobility and lifestyle for a growing segment of the population.
“We are a ways from bringing these treatments to patients,” says Sankaran, “but Duke’s investments in basic science and in the applications of regenerative medicine are how these ideas will become reality.”
For more information, visit Regeneration Next Initiative.