Those who remember the crash test dummy commercials for automobiles in the 1980s know that testing new technologies using human models first can help keep actual people safe.
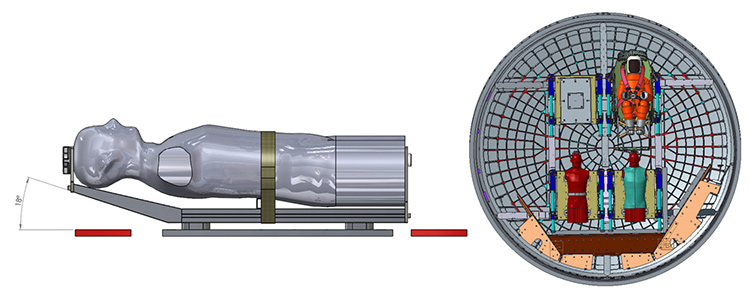
In 2020, two life-like human models—or ‘phantoms’ as researchers call them— will be strapped into NASA’s Orion spacecraft and flown to the moon and back. They’ll be fitted with more than 1,400 sensors in order to measure radiation exposure as they travel through space.
The mission is a collaboration between the German Aerospace Center, NASA, and the Israeli Space Agency to investigate the radiation exposure experienced by astronauts on deeper space travels. The project will mark the first time that scientists collect data on radiation exposure beyond the orbit of the international space station. The ultimate goal is to explore the possibility of sending humans to Mars.
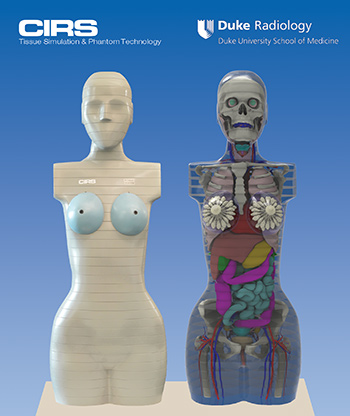
Paul Segars, PhD, associate professor of radiology, and Ehsan Samei, PhD, professor of radiology, both researchers at the Carl E. Ravin Advanced Imaging Laboratories at the Duke University School of Medicine, worked with manufacturing companyCIRS to develop the phantoms. Segars and Samei defined mathematical models for the interior anatomy of the phantoms that allows them to calculate radiation exposure to individual organs. The models were originally created to investigate medical procedures, but they are also useful for measuring a person’s exposure to radiation in other environments, including space.
“There are all sorts of risks involved in a space mission, and radiation exposure is just one of them,” said Samei. “What’s important when calculating risk to a patient or to an astronaut is not how much total radiation dose is received, but how much dose is received to individual organs such as the brain, heart, liver, and kidneys. It matters how it spreads out because each organ has a different sensitivity to radiation.”
For example, breasts are especially sensitive to radiation, while other organs, such as the pancreas, typically are impacted less, said Samei. The human models that will be sent to the moon next year will both have female anatomies. One of the models will be wearing a protective vest to test whether it is successful in blocking radiation. The protective shield vest, called the AstroRad, was developed by StemRad, in conjunction with Lockheed Martin
Sending female models is important because it demonstrates the worst-case radiation exposure; women are more sensitive to radiation than men. Although the difference is well established, the cause is not completely certain, with some conjecturing that it could be due to gender hormonal factors, said Samei.
Progress has been made in the past few decades to advance the use of human computational models in practice, and Segars and Samei have been working for the past ten years to perfect their models. The anatomical models utilized for this project arose out of their work in creating a population of ‘virtual’ patient models or phantoms for medical imaging research
The virtual patients, which provide highly detailed representations of the human body and physiology, can be combined with accurate simulation techniques that mimic medical procedures including imaging to perform ‘clinical’ experiments entirely on the computer. Different procedures can be simulated, and the results are analyzed and compared to the baseline data provided by the computational models.
“The phantoms and simulation tools provide an efficient means with which to quantitatively evaluate, optimize, and compare medical devices and techniques. They give you a way to perform experiments that would be otherwise impossible with live subjects,” said Segars.
As research continues to advance in the area of human computational modeling, Samei said his hope is that human computational models will be integrated more often into clinical practice. “Our challenge in medicine is that science relies on experiments to advance knowledge and to improve care to our patients, but very few such experiments are ethically allowed in medicine, rightly so,” said Samei. “So, our goal here was to create a new paradigm in which we have these virtual patients that we can use, perhaps not to the exact realism of human patients but close enough and much better than more simplistic models. We have verified in multiple instances that our virtual enterprise is predictive of what happens in actual clinical practice.”
And beyond clinical practice to the final frontier, the work of Drs. Segars and Samei have led to a dream come true project.
“As a kid growing up watching Star Trek and Star Wars, you always dream of doing something in outer space,” said Segars. “It’s exciting to think that these phantoms will travel through space and will help pave the way for future exploration.”