
When Shelley Hwang, MD, MPH, is in the operating room performing surgery on a patient with breast cancer, she focuses all of her considerable experience, skill, and knowledge on the task at hand: giving this individual patient the best possible outcome. At the same time, she recognizes that every operation is an opportunity to learn just a little bit more about the disease she battles every day. Every patient and every procedure add to the store of knowledge that guides research and ultimately informs the advances that improve care.
“Surgeons are on the front lines against disease,” says Hwang, the Mary and Deryl Hart Distinguished Professor of Surgery and vice chair of research at Duke University School of Medicine. “Who is in a better position to understand the enemy? We are a clinical discipline, and clinical care is always going to be the most important thing we do: our first obligation is to the patients we have now. But we are also in a rare position to make a difference for all those patients we are never going to meet in person."
"We can contribute to patients’ health on an individual level, but we can also contribute to the knowledge base and improve human health worldwide. What an incredible privilege that is. That’s the beauty of research.” 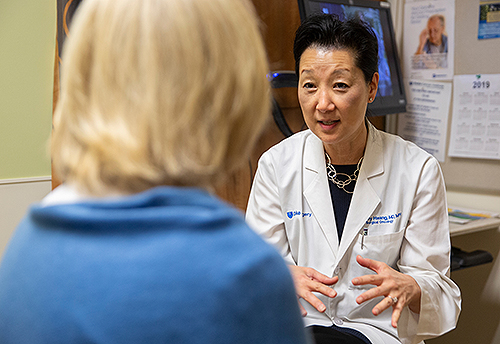
-Shelley Hwang, MD, MPH
Duke University's Section of Surgical Disciplines, which comprises the Department of Surgery and the Department of Head and Neck Surgery & Communication Sciences, achieves excellence both in providing first-rate clinical care and in conducting groundbreaking research at an exceptionally high level. Duke Surgery is ranked in the top four nationally in both the U.S. News & World Report overall rankings and in National Institutes of Health research funding. The section has ranked in the top five in NIH research funding for the last 11 fiscal years, reaching No. 1 in 2018, and Hwang was the nation’s top NIH-funded individual surgeon-scientist that year.
In addition to performing some 80,000 surgeries every year, the 326 faculty members in the Section of Surgical Disciplines conduct over 400 clinical trials and publish more than 500 papers in peer-reviewed journals annually.
Very few academic surgical departments are able to balance the demands of the operating room and the research lab at such high levels of achievement. At many institutions, time constraints, pressure to maintain high volumes of procedures, and funding limitations keep surgery and research all but mutually exclusive.
One key to balancing clinical care and research, says Allan Kirk, MD’87, PhD’92, HS’95, vice dean of the Section of Surgical Disciplines, is treating them not as two different missions, but as two aspects of the same one. At Duke, not only are surgery and research not mutually exclusive: they’re mutually supportive. Surgical practice informs research, and research leads to innovations and improvements in surgical practice.
“Doing surgery gives you insights and data that inform your investigation as a researcher that you couldn’t get otherwise,” says Kirk, the David C. Sabiston Jr. Distinguished Professor of Surgery. “We help our surgeons find areas of research that are facilitated by their surgical practice and patients. If you’re a heart transplant surgeon and you’re interested in heart transplant biology, your surgery gives you a leg up over researchers who can’t do surgery. We look for areas of research where there’s a synergy between clinical practice and discovery. Then your role as a surgeon is a competitive advantage, not an impediment.”
A CULTURE OF DISCOVERY
When Kirk came to Duke in 2014 from Emory University, one of the things that drew him here was the commitment within the School of Medicine and the university to excellence in research as well as clinical care. Essential to success is enthusiastic buy-in from university administration, School of Medicine Dean Mary E. Klotman, BS’76, MD’80, HS’80-’83, HS’83-’85, and departmental faculty.
“Everyone I spoke to, at every level, wanted surgeons to be a part of discovery,” says Kirk. “That is very rare. Most health centers see surgery as maybe financing the discovery mission, but not being an active part of it. At Duke, nobody thinks surgery should be anything other than an active part of discovery. The institution wants surgeons to be involved in discovery, and the surgeons want to be involved in discovery. Once you have that level of commitment, it’s just a matter of logistically making it work.”
The department has created an impressive infrastructure to support the entire research spectrum, from basic science to clinical implementation and everything in between. Kent Weinhold, PhD, is chief of the Division of Surgical Sciences, a unique division where basic and translational scientists work on everything from molecular immunology to gene therapy to wound healing. The Surgery Office of Clinical Research, under Julie Thacker, MD, coordinates clinical research aimed at improving patient safety and therapeutic effectiveness. The Surgical Center for Outcomes Research, led by Chuck Scales, MD’04, HS ’05-‘11, is a health service research unit that uses various methodologies to assess factors that affect surgical outcomes. Shared resources such as the Substrate Services Core Research Support serve as biorepositories for data and sample storage and analysis, saving money and achieving efficiencies of scale.
Weinhold, the Joseph W. and Dorothy W. Beard Distinguished Professor of Experimental Surgery, says the Division of Surgical Sciences—and, indeed, the entire culture of discovery in the Division of Surgical Sciences—is a legacy of David Sabiston, MD, the legendary chair of surgery from 1964 to 1994, and his predecessor, Deryl Hart, MD.
Hart established the Division of Experimental Surgery, the forerunner of the Surgical Sciences Division, and Sabiston made basic science a fundamental component of the department’s mission, integrating discovery and patient care and requiring that surgical residents spend 2-3 years doing basic research.
“Dr. Sabiston believed an academic surgeon should be one who is not only extraordinarily gifted in the operating room, but one who is equally gifted at doing hypothesis-driven research and moving the field forward,” says Weinhold, whom Sabiston recruited in 1980.
“He recruited a number of outstanding basic scientists and entrenched them with the clinical faculty to encourage new ideas and collaborations. And that’s still the ethos here. I don’t think I’ve ever approached a clinician here with an idea for a project and had them say no. It’s always, ‘That sounds interesting. Let’s give it a try.’”
-Kent Weinhold, PhD, on David Sabiston, MD
1KP
Among the most innovative and far-reaching research programs launched within the Section of Surgical Disciplines is the 1000 Patient Project, known informally as “1KP.”
The 1000 Patient Project is based on the premise that surgery is, in essence, a planned, highly controlled form of injury—and therefore an opportunity to study injury and recovery.
Dozens of Duke surgeons work together with the 1KP research team to gather detailed physiological, demo-graphic, genetic, immunological, and other data from patients undergoing any one of 12 different types of surgery. This wealth of information offers unprecedented insights into a vast range of questions: How do various systems and processes react to trauma? What constitutes resilience? What factors impede recovery, or improve it?
“Our bodies constantly work hard to maintain homeostasis,” says Hwang. “This gives us a chance to look deeply at what happens when we perturb that process. What happens to their genes? What happens with their stress proteins or immune system? Are we altering their biome, and how does that influence recovery? How do all these systems work to return to homeostasis?”
Those answers, in turn, can lead to new therapies and new approaches.
“We want to use this data to identify biomarkers that will help us predict how well individual patients will do, and to develop interventions to increase resilience and recovery,” says Hwang. “This is our big departmental science project. It’s touched pretty much every surgeon in our departments in some way, and we are grateful to the hundreds of enthusiastic patients who have volunteered critical samples and time to this effort.”
The section has created infrastructure to store and sort the huge amount of data generated by the 1000 Patient Project. Researchers are tapping that data for myriad projects.
“Side projects are firing out all over the place,” says Kirk. “The 1000 Patient Project has already gotten a lot of translational and clinical research projects off the ground. It also has given the whole department a project it could work on collectively, and that has helped discovery permeate into a lot of new areas.”
A BLACK BOX FOR THE OR
The flip side of 1KP is a new project the section calls the “OR Black Box.” The idea, pioneered by Teodore Grancharov, MD, at St. Michael’s Hospital on Toronto, is based on the ubiquitous “black box” systems that record flight data during every commercial airline trip. If a plane has a problem, investigators can analyze the data stored on the black box to determine what went wrong.
In the operating room, the Black Box system will place audio and video recorders to capture the activity during each operation. Correlating that activity with outcomes will guide improvements in surgical efficiency, patient safety, and results.
While the 1000 Patient Project gathers data on the physiological factors that affect recovery, the Black Box project will provide insights into external factors that may influence outcomes—some of them not immediately obvious.
“The Black Box is going to tell us a great deal,” says Julie Thacker, medical director of the Clinical Research Unit, which is overseeing the project. “How many times does the door open and close? How many times was the surgeon interrupted? Does a procedure get delayed if someone has to leave the room to get an instrument? Do these things tend to happen at certain times of day? Are the interactions among the surgical team efficient and natural, or tense and difficult? And so on. All of these things can potentially affect outcomes.”
For example, a 2015 study at Johns Hopkins found that operating room doors opened an average of once every two and a half minutes during surgery. Every time that happens, air flow and pressure can change and contaminated air from outside has the potential to enter the room, possibly affecting rates of infection.
Another facet of the Black Box program involves in-device cameras that record robotic laparoscopic surgeries.
“The point is to examine how we do things and look for ways to do them better,” says Thacker. “We have great doctors and nurses. But until somebody comes up with a way to do perfectly painless, perfectly non-intrusive operations, there is always room for improvement.”
HOLDING DISEASE IN THEIR HANDS
As Dr. Sabiston recognized half a century ago, few people are more intimately familiar with disease than surgeons, and that gives them a special responsibility to explore it. The philosophy of discovery he instilled continues to drive the department.
“To surgeons, disease is not an abstract concept,” Kirk says. “It’s something we are literally immersed in. We hold it in our hands. And that tactile immediacy gives you the desire to understand disease at a deeper level, to learn things that you can use to improve care.”
The surgeons at Duke are engaged in that work on countless fronts. Technology has enabled clinicians and researchers to collect vast amounts of data, fueling discovery at every level, from molecular genetics to population health.
Discovery is expensive. Federal funding, of course, is essential, but Kirk says philanthropy plays an increasingly important role as well.
“Doing anything well costs money,” he says. “Doing it poorly costs more. We have made great strides toward building the best academic Section of Surgical Disciplines that we can. As margins decrease, we are going to become increasingly dependent on philanthropy to continue this work.”
And as they do, Kirk says, they keep one person always in mind.
“We capture huge amounts of data, and we explore all kinds of questions, but all of it links back to the people we treat,” he says. “The key factor is to keep the patient at the center of everything we do.”