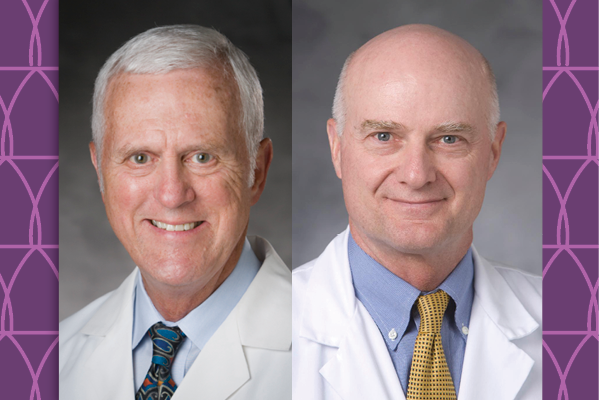
As Duke University prepared to celebrate its centennial, and Duke Cancer Institute marked its 50-year anniversary, two Duke cancer physicians and 1973 Duke University Medical School alumni hung up their coats after providing 50 years of compassionate care.
On December 31, 2023, 50 years to the day after he began his residency at Duke University School of Medicine, medical oncologist William Berry, MD, clinical associate in the Department of Medicine, retired from caring for Duke Raleigh patients with prostate, kidney, bladder, and testicular cancer.
On July 1, 2023, plastic surgeon and surgical oncologist Gregory Georgiade, MD, professor of surgery, retired from clinical practice after 50 years, all of them spent at Duke. Georgiade had also held many additional leadership roles in Duke University Hospital, some of which he will continue until successors are found.
Changing the Landscape for Prostate Cancer
In 1979, when Berry started his private hematology-oncology practice in Raleigh, North Carolina, he didn’t treat prostate cancer patients because there were no approved medical therapies to offer them. Today, as he begins retirement, there are so many approved drugs for men with prostate cancer, many of which he had a hand in testing, that for the last 20 years he has focused his practice solely on these patents.

Berry began and ended his career at Duke. After medical school here, he stayed for an internal medicine internship and residency, which led him to fall in love with oncology, which he calls an “emotionally intense” specialty. “It was pretty remarkable what you could do to make a cancer regress or make a leukemia go into remission with drug therapy,” Berry said. “Sometimes patients don’t do as well as you or they would like. That part of it can be hard. But the rewards of helping people outweighed the drawbacks.” Barry recalled many Duke mentors who “helped him get things done,” including Harold Silberman, MD, the first oncologist he ever worked with.
Berry had conducted research on prostate cancer during his fellowship, but in the beginning of his practice, he treated leukemia and other cancers for which he could offer medical therapy. In the mid-1990s he began helping change the landscape of treatment for men with prostate cancer, enrolling patients in clinical trials for targeted therapies, and serving as chair of the Genitourinary Research Committee for U.S. Oncology (a national network of oncology practices).
“It was an exciting time in prostate cancer, getting in on the ground floor. There weren’t that many people involved,” he said.
Berry was diagnosed with the disease himself in 2001. “I've done well and haven't had any recurrence, but that just kind of cemented it,” he said. Having that experience himself built rapport with his patients, and he transitioned his work to focus almost exclusively on prostate cancer. In 2014, Berry’s practice became part of Duke Health, and he joined the faculty at his alma mater.
“Bill Berry has been a giant in the field of advanced prostate cancer therapies, starting with mitoxantrone and docetaxel chemotherapy decades ago and evolving into more targeted immunotherapies and hormonal agents recently,” said Andrew Armstrong, MD, professor of medicine. “He is a fierce patient advocate and great collaborator, and it has been a privilege to have him here at Duke the past 10 years.”
As he transitions to retirement, Berry said he looks forward to spending more time traveling with his wife, visiting their grandchildren (two four-year-old boys and a one-year-old girl), and working in his vegetable garden and rock garden (cacti, agave, and yucca).
A Master Surgeon and More
Gregory Georgiade, MD, professor of surgery, who was born at Duke University Hospital, likes to call himself a “Duke lifer.” “They don’t give neonates a life sentence, but I got one of them,” he said. His father, Nicholas Georgiade, MD, was a plastic surgeon and chief of the division of plastic surgery at Duke, and by age 13, the younger Georgiade was observing him in the operating room. Just before college at UNC-Chapel Hill, he participated in a summer internship during which he had the chance to serve as a “scrub tech.”
Once enrolled at Duke medical school, Georgiade considered other specialties but found he liked plastic surgery because of the ability to make a big difference in a short amount of time for patients, such as a person with traumatic injuries or a baby with a cleft lip. “There are some procedures where an hour and a half could make dramatic changes in someone’s life,” he said. “That attracted me as opposed to internal medicine where you’re often treating a long-term disease process.”
Georgiade’s work has spanned not only surgical oncology but also general surgery, trauma surgery, maxillofacial surgery, and cleft lip and palate surgery. “My definition of plastic surgery is broad: the skin and all its contents,” he said. He is one of the few people at Duke recognized by his peers as a master surgeon, in recognition of exceptional contributions to Duke Surgery.
“It is impossible to categorize Greg Georgiade as belonging to any single surgical specialty, as no specialty encompasses the breadth of skill he has mastered,” said Allan Kirk, MD, chair of the Duke Department of Surgery. “He is technically comfortable anywhere in the body, possesses the decision-making skills required by complex elective reconstructions through catastrophic emergency procedures, and has achieved and contributed to pragmatic and routine operations as well as to newly imagined areas of discovery. He is simply a surgeon’s surgeon in the very best sense. He has inspired generations of trainees, including myself, and his legacy will continue to be a source of inspiration for our department and our institution.”
Among Georgiade’s many research contributions is a seminal 1984 study reporting the first set of outcomes data showing that immediate reconstruction after mastectomy did not worsen disease progression or cause recurrence or cause undue complications, opening new avenues for patients.
Georgiade said he is grateful for the breadth of opportunities he has had to become involved in the health system outside of the operating room. In 1985, he helped establish Duke Life Flight, the first hospital-based transport service in North Carolina, and he has served as its medical director since then. In 1998 he led the creation of the Duke Aesthetic Center and still serves as its medical director, and he serves as director of the Human Fresh Tissue Lab (a surgical training lab). He will continue to serve in those roles until successors are found. He previously served in other leadership roles at Duke University Hospital, as well as chief of the Department of Surgery’s division of plastic, maxillofacial, and oral surgery.
Georgiade said that retaining his nurses and administrative team has been critical to his success. “Without the people working around me taking care of the needs of patients and referring physicians, I couldn’t have delivered the care I was able to deliver.” His current nurse had worked with him for 15 years. “When patients come to see the name nurse for 15 years, the visit becomes a social event. It makes it a welcoming environment. People can get their care elsewhere, but they come here because the team knows who they are,” he said.
Georgiade seems to have been destined to be a surgeon, but if he had pursued any other career, it would have been something outdoors, he said. He looks forward to spending more time in nature, including visiting his grandchildren and son, who runs a wilderness canoe camp in Canada.