
Rodger Liddle Has A Gut Feeling About the Origins of Parkinson's Disease
What is a gastroenterologist doing studying Parkinson’s Disease?
This is a question that Rodger Liddle, MD, a professor in the Department of Medicine in the School of Medicine, gets a lot. The answer involves a superhighway, a conversation with a Nobel Laureate, and a plastic foot.
Liddle usually begins the story with the foot.
In his office, carefully situated on a bookshelf among anatomy books, photos from medical school, and colorful knickknacks from international travels, sits the slime-green foot. Approximately five inches long, with an elongated toe bed and a skinny ankle, it almost resembles the snout of a crocodile.
However, to Liddle, it will always look like a foot because it reminds him of the moment that his career took a step in an entirely different direction.
“This is a neuropod,” he explains, holding the plastic 3D-printed model at arm’s length. The strangely shaped cell was discovered by Rashmi Chandra, PhD, and Diego Bohórquez, PhD, in 2011. At the time, Chandra was a long standing member of the Liddle laboratory and Bohórquez was a postdoctoral fellow in his laboratory. They discovered this cell using a confocal microscope to examine the cells that line the gut wall of a mouse.

For years Liddle has studied how hormones in the gut work. One hormone in particular called cholecystokinin, or CCK, lines the gut wall and is released when cells are jostled around by food. CCK travels through the bloodstream, stimulating digestion and letting the brain know whether the stomach is full and satisfied.
Scientists have long accepted that this process was a conduit for the gut’s connection to the brain. But the cell that the team saw under the microscope that day was different from all the others they’d previously seen hanging out in the gut.
Three years later, in 2014, Bohórquez used electron microscopy to get a 3D image of the cell, and what he saw surprised him. For starters, the cell had neurofilaments, which are typically found in the axons of neurons, or nerve cells – and not normally found in the gut. Secondly, the cell had small clear secretory vesicles, resembling those in neurons that contain neurotransmitters—also not normally found in the gut. On top of that, it was also packed with mitochondria, meaning it required energy. And it had synaptic proteins.
Bohórquez, who trained in the Neurosciences at Duke and the Marine Biological Laboratory, performed other experiments to test this finding. He reached out to colleagues in the Department of Neurobiology including Nicole Calakos, MD, PhD; Marguerita Klein; and Fan Wang, PhD, for guidance.
Wang suggested that he inject rabies virus, a virus that only infects nerve cells, into the gut of a mouse. If the cell in the gut was infected by rabies, it would imply that it was a nerve-like cell. If the rabies virus spread onto an adjacent nerve, it would prove the gut cell was connected by a synapse with the nerve.
Bohórquez injected the virus and found just that - proof that there was a direct circuit—a neurocircuit—between the gut surface and nerves.
Next, he conducted another experiment often called “Two Brains in a Dish” in which a gut cell and a nerve cell were placed into a petri dish together. Within 24 hours, the cells had moved toward one another, touched and then the gut cell withdrew with a connection between them.
The discovery threw Liddle and Bohórquez for a loop. It suggested a quicker, faster connection between the gut surface and the nervous system, the difference between a superhighway and a slow-moving train.
“We couldn’t contain our excitement,” said Bohórquez. “The term ‘gut feeling’ had always been esoteric but we were uncovering the basis of a very direct link between the gut and the brain.”
Their discovery was published in the Journal of Clinical Investigation in 2015. From there, the possibilities for new research ventures seemed endless.
Bohórquez, who is now an Assistant Professor of Medicine and Neurobiology at Duke, discovered in his laboratory that these cells form a neural circuit conveys signals from nutrients in the gut to the brain in milliseconds. He named these cells neuropod cells. His laboratory studies how the gut senses the caloric value of nutrients to influence the choice of food we eat.
Liddle went another route.
“As a physician, I thought, well what does this mean for disease? Are there diseases that could be related to this process?” said Liddle. One immediately came to mind: mad cow disease.
Most people associate mad cow disease with the outbreak that occurred in the late 1990s in the United Kingdom, when a fatal brain disease in humans called variant Creutzfeldt-Jakob disease (vCJD) was linked to consumption of cattle that had been sick with bovine spongiform encephalopathy (BSE), a neurological disease in cows. Patients experienced movement deficits, memory disturbances and cognitive impairments.

Liddle wondered if prions, the infectious proteins discovered in the cow meat, had used the gut-brain connection to infect humans with the disease. He knew exactly who he needed to talk to: Stanley Prusiner, a neurologist at the University of California San Francisco who won the Nobel Prize in 1997 for his discovery of prions.
In a stroke of luck, Prusiner was already planning to give a talk at Duke, so Liddle set up a meeting with him during his visit. He remembers their conversation like it was yesterday, and with a chuckle. It went something like this:
Liddle: Stan, I think this is how you get mad cow disease.
Prusiner: I think you may be right.
Liddle: Would you like to work on this together?
Prusiner: No.
Liddle: Stan, what are you talking about? You won the Nobel prize for discovering prions, and this is how you might get mad cow disease and nobody knows how you get mad cow disease… don’t you want to work on this together?
Prusiner: No.
Liddle: Why?
Prusiner: When was the last time you saw a patient with mad cow disease? And when was the last time I took a vacation?
Prusiner was overloaded with work and couldn’t commit to another project. But Liddle thought long and hard—it was true, he had never seen a patient with mad cow disease. The disease is extremely rare. Prusiner, however, had another suggestion: Parkinson’s disease.
“And I go— Parkinson’s disease!? I’m a gastroenterologist. What do I know about Parkinson’s disease and what does it have to do with this? And he says no, no, no, there’s evidence that Parkinson’s disease may be a prion disease and maybe it starts in the gut. So I say, well okay, and I start to read about Parkinson’s disease. And sure enough, there’s some evidence that Parkinson’s might start in the gut,” said Liddle.
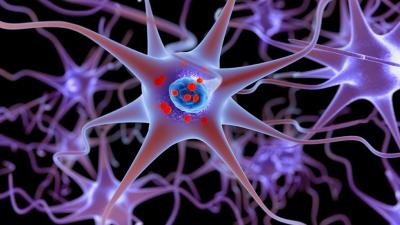
In his research, Liddle found that a hallmark of Parkinson’s disease is Lewy bodies, which are abnormal aggregates of proteins that develop inside nerve cells. One of the major proteins found in Lewy bodies is called alpha-synuclein. Chandra ran some experiments and determined that the recently discovered cells that have neuropods actually contain the gene that encodes for the alpha-synuclein protein. Therefore, the same types of cells that can make Lewy bodies that cause Parkinson’s Disease are made in the gut.
Liddle wondered: Is it possible that the Lewy bodies use the superhighway from the gut to the brain to get to the brain, where they cause disease?
If it’s found that they do, it could explain a lot. In the clinic, ten percent of Parkinson’s disease cases are linked to hereditary causes, but an overwhelming 90 percent are sporadic with unknown causes.
Liddle, who sees patients with all sorts of gastrointestinal illnesses, has noticed in his own clinic that patients with Parkinson’s disease often have constipation that develops before they’re ever diagnosed with the neurological disease.
“Some patients will develop constipation ten years before they ever have the tremor and the clinical manifestations of Parkinson’s disease,” said Liddle. “Or they might develop problems with their stomach emptying, a condition caused gastroparesis which is due to Parkinson’s disease affecting their stomach. So it’s another piece of evidence to suggest it might start in the gut.”
There are historical links as well. During the Vietnam War, soldiers exposed to Agent Orange, a tactical herbicide used by the U.S. Military, were shown to have a higher incidence of Parkinson’s disease. Meanwhile, people near a water contamination site in Camp Lejeune, North Carolina from the 1950s to 1980s were shown to have higher incidences of Parkinson’s disease.
Liddle suspects that exposure to certain chemicals through ingestion is what may play a part in the formation of Lewy bodies in the gut, which then spread to the brain, causing Parkinson’s disease. But much more research is needed before researchers can say for sure.
“We think Parkinson’s disease starts in enteroendocrine cells where alpha-synuclein becomes deranged,” said Liddle. “From there it can spread into the nervous system. If we find that these cells are the origin of Parkinson’s disease, it could provide a way for preventing it.”
“If five years ago you told me I would be working on Parkinson’s disease, I would not have believed it,” he added. “Every step has been one surprise after another.”
Watch Dr. Liddle explain his research for the Duke GI Oral Histories Project:
Listen to Dr. Liddle explain his research on the Voices of Medicine Podcast:
Top image in story: 3D illustration showing neurons containing Lewy bodies small red spheres which are deposits of proteins (alpha-synuclein) accumulated in the brain cells. iStock.
Lindsay Key is the science writer for the Duke University School of Medicine, and editor of the online storytelling magazine Magnify.