

Listening in on the Conversations of Fat Cells
Your body is in constant dialogue with its own fat, and fat talks a lot.
Understanding those conversations and trying to get a word in edgewise is the focus of Duke Science and Technology scholar Rana Gupta, PhD, a professor of medicine at Duke University School of Medicine and a member of the Duke Molecular Physiology Institute.
“Your fat tissue is not just an energy bank, it's not just an energy furnace,” Gupta says in his Carmichael Building office overlooking the pickup lane at the Durham School of the Arts. “It's a very talkative, chatty tissue and it’s like an immunological organ.”
Identifying all the parties of this cellular conversation and perhaps learning to interrupt them is where Gupta’s research path has led. Why do we only make fat in certain places, and why is that different between men and women? How can we make more fat cells to avoid having bigger fat cells? How can we keep the liver and the fat on healthy speaking terms and avoid glucose intolerance?
“How fat expands and where it expands is going to be the big determinant of your metabolic health,” says Gupta, who joined Duke this year from the University of Texas Southwest Medical Center in Dallas.
Origin Stories
Gupta’s undergraduate and graduate training were in biochemistry and pharmacology, respectively, at the University of Pennsylvania. “It was really two things that motivated me, and still motivate me today: One is developmental biology: Where do we come from? Where do all of our cells come from? How do we go from egg and sperm to who we are?” The other fascination, driven in part by his own immigrant family’s experience, was diabetes. “So, I joined a lab studying pancreas development with the goal of regenerating insulin-producing beta cells.”
For his postdoctoral research at the Dana Farber Cancer Institute at Harvard, Gupta switched the focus slightly to look at obesity’s connection to diabetes.
“What I was really struck by is that you have a tissue — fat — that can just expand like crazy. It’s almost unparalleled in our body to have a tissue that can expand and contract in size like that.” At the time, nobody quite knew where fat cells came from — that is, what their version of a stem cell might be. Gupta and others now know there isn’t only one answer to that question.
“The way we think about this now is that the fat tissues in different parts of the body are really just different organs altogether,” Gupta says. “So, we don't just have fat tissue, we have different types of fat cells coming from different precursors. And they're defined basically by where they are in the body.”
What’s in a Color
We have fat because it’s useful. Or at least it was when we were less certain of finding a 1,500-calorie meal around every corner. Fat is the bank where we store excess energy to tide us over. All of this is normal, unless you’re consistently taking in more energy than you can burn.
“The healthier your fat tissue is, the better ability it has to talk,” Gupta says. “What often happens as one develops obesity, is that the fat tissue gets bigger and bigger and then it becomes dysfunctional.”
White fat and brown fat, you may have heard of. Brown fat is like the furnace — it appears brown because of a heavy accumulation of fuel-burning mitochondria. This is where stored energy becomes useable energy. White fat is like the coal pile, bits of which are released into the blood stream to be burned up by the brown fat cells.
For the most part, adults have barely detectable amounts of brown fat, usually concentrated around the neck and shoulder blades. Newborns have a lot of brown fat in this area, but in adults it’s largely invisible, and for decades scientists assumed it was unimportant because it went away. Only in 2008 did somebody identify brown fat in adults and begin to tease apart its role.
Gupta also studies something called beige fat that is between the two in both appearance and function and can flip back and forth between their different roles. Perhaps controlling beige fat will help us, he says.
Breakdown
What Gupta and other fat-whisperers would like to understand better now is where all these different kinds of fat cells come from and how they are maintained. Each kind of fat has its own precursor cells, and unlike other cells, fat cells don’t divide to copy themselves, each coming from a precursor.
What fat cells also do that’s different is dramatically change their individual sizes — fat cells themselves get fatter. They swell in response to the continual oversupply of energy.
The way metabolism researchers see it now, the issue in diabetes isn’t the deposition of extra energy from the diet being put into those swelling fat cells — that’s what we’re meant to do — but what happens after that as the fatty diet continues.
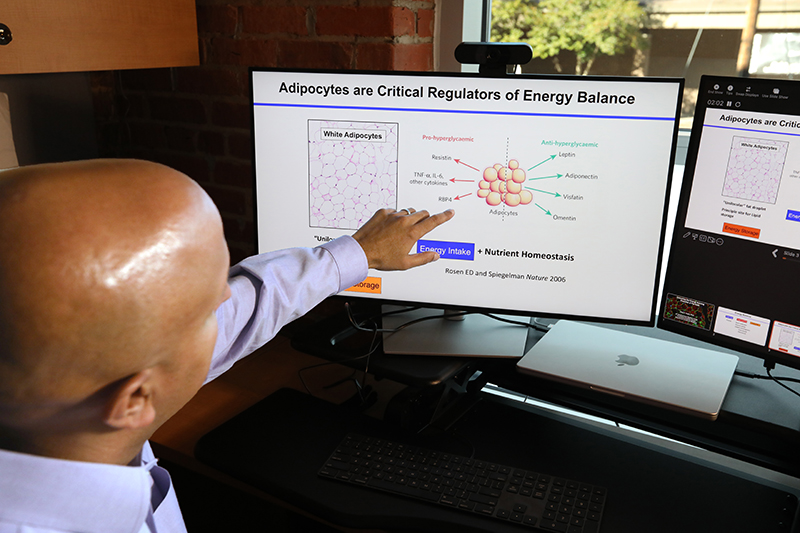
Gupta pulls up a slide on his monitor — fat cells in an obese mouse with insulin resistance. The cells are quite large and surrounded by blue tendrils. “That blue stuff is all immune cells,” Gupta says. “These are dying fat cells that are being chewed up by these immune cells, and so we get a lot of inflammation.”
“At some point, these fat cells just break down, they can't handle it anymore,” Gupta says. “You've asked them to do too much. And that leads to cell death, inflammation, and something called fibrosis, which is a sort of scarring.”
Gupta says that fat-driven inflammation, in turn, helps explain the success of some cancers, which thrive on inflammation and feed on fats, and the higher mortality rate of obese people who contracted COVID-19.
If you’re still eating more than you’re burning, the fat is going to spill over and damage other tissues. “It's strongly believed now that's how we get diabetes,” Gupta says. “It’s because we have now disrupted the function of your skeletal muscle and your liver, so that you can no longer handle glucose properly.”
Then the question becomes: “Could we fix the fat so that it works?”
Fixing the Fat
One thing Gupta’s lab has tried is signaling fat cell precursors to crank out more fat cells to avoid making fat cells bigger. The mice in this experiment ended up with better metabolic health as a result. And there might also be a way to encourage white cells to become beige or brown, Gupta says.
Another discovery from his lab is a transcription factor — a molecule that tells genes what to do — that sends the signal to a developing fat cell that it should be white, not brown. Deleting that transcription factor from fat cells led to them turning brown. “We can also remove it from an obese mouse and make it lose weight and reverse its glucose problems.”
Is a miracle drug on the horizon? “We're not there yet where we can identify the best drug targets,” Gupta says. “I think we're still in the stages where we're identifying the mechanisms, just learning how the system naturally works. Can we use stem cell biology as a way of fixing the fat to improve metabolic health?”
Karl Leif Bates is the Director of Research Communications at Duke University.
Photography by Jim Rogalski, senior video and multimedia producer, Duke University School of Medicine Office of Strategic Communications
Main photo: Rana Gupta, PhD, a professor of medicine in the Division of Endocrinology at the Duke School of Medicine and member of the Duke Molecular Physiology Institute, studies metabolism.